Lung Cancer: Who is a Candidate for Surgery?
Chest X-ray
The standard chest x-ray is useful in detecting the primary tumor and demonstrating its size and location but is not sensitive (the likelihood that a test will be positive in patients who have the disease) in detecting lymph node involvement. Chest x-ray may show a pleural effusion, destruction of ribs or vertebrae, and involvement of the phrenic nerve with elevation of the hemidiaphragm. Chest x-ray is inferior to CT in evaluating mediastinal nodal disease. If suspected mediastinal involvement on x-ray is found, more accurate imaging studies should be obtained.
Computed Tomography (CT)
CT localizes the primary tumor and allows characterization of its size and relationship to adjacent structures as well as involvement of hilar and mediastinal lymph nodes, with those larger than 1 cm considered abnormal. Contrast-enhanced helical CT of the chest and abdomen are routinely performed to evaluate for metastases to the liver and adrenal glands. Nonresectable lesions include those involving the carina (the junction of the right and left mainstem bronchi) and tumors surrounding the aorta, the main portions of the pulmonary arteries, or more than 180 degrees of the esophagus. CT is useful in guiding further biopsies using mediastinoscopy or VATS. However, CT is only 57% sensitive and 82% specific (the likelihood that a test will be negative in patients who do not have the disease) for detecting positive mediastinal nodes (5), and inflammation can lead to under or over-staging. In addition, nodal metastases can be present in 21% of nodes less than 1 cm in size (3). Magnetic resonance imaging (MRI) has a similar sensitivity and specificity to CT but does not require contrast. However, spatial resolution is inferior to CT, and the images are limited by cardiac and respiratory motion artifacts.
Bronchoscopy
Bronchoscopy can be used to define the proximal extent of the tumor. Bronchoscopic signs that a lesion is not resectable include vocal cord paralysis suggesting nerve invasion and tumor involving the carina or trachea. Lymph node invasion can be evaluated using transbronchial needle aspiration by passing a needle through the bronchoscope and the bronchial wall into the lymph node. However, sensitivity is only 50% with a 96% specificity (3).
Mediastinoscopy
When radiologic studies are inconclusive or enlarged mediastinal lymph nodes greater than 1 cm are present, surgical techniques including cervical mediastinoscopy (Figure 2), anterior mediastinotomy (through a small anterior chest incision), and thoracoscopy are used to evaluate lymph node involvement.
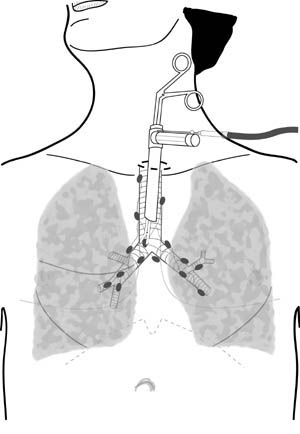 Figure 2. Illustration demonstrating cervical mediastinoscopy to evaluate lymph node involvement by lung cancer
Figure 2. Illustration demonstrating cervical mediastinoscopy to evaluate lymph node involvement by lung cancer
Mediastinoscopy is the gold standard for mediastinal staging with an 89% sensitivity and 100% specificity for non-small cell lung cancer. Only 8% of patients with a negative mediastinoscopy were found to have mediastinal nodal disease at exploration (6). The sensitivity may be improved in the future by using techniques that can better identify microscopic disease, such as molecular methods to detect the presence of tumor RNA or proteins. Cervical mediastinoscopy can be performed as an outpatient procedure with minimal complications. Anterior mediastinotomy or VATS can be used to evaluate lymph nodes that are less accessible by mediastinoscopy, particularly nodes in the left chest. VATS (Figure 3) can also be used to exclude a malignant pleural effusion in patients who would otherwise be candidates for complete surgical resection.
 Figure 3. Pleural nodule discovered during video-assisted thoracic surgery.
Figure 3. Pleural nodule discovered during video-assisted thoracic surgery.