Health Centers > Cancer Health Center > Vulvar Cancer
Vulvar Cancer
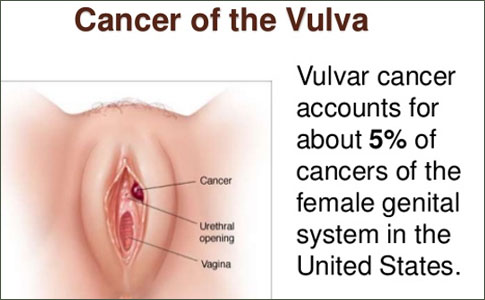
Vulvar cancer is an uncommon malignancy, responsible for only 5% of all gynecologic neoplasms, but its incidence is on the rise. Although the age of onset of vulvar cancer varies widely, most cases occur in women over age 50. Peak incidence occurs between the ages of 65to 70.
Epidemiologic studies have shown associations between vulvar cancer and genital warts, abnormal Pap smears, and smoking. Molecular analysis of vulvar neoplasias has revealed the presence of human papillomavirus (HPV) genomic material. These findings support an etiologic relationship between papillomavirus and vulvar cancer. Vulvar intraepithelial neoplasia (VIN) predisposes to vulvar cancer. Lichen sclerosis is not generally considered to be a premalignant condition. Squamous cell hyperplasia is often found in regions adjacent to vulvar cancer, but the relationship of this lesion to invasive cancer is unclear. Advanced age and race (white) have been shown to be independent predictors of poor outcome.
Although it seems intuitive that vulvar cancer would be relatively easy to diagnose because of the accessibility of the vulva to visual inspection, clinical findings may be subtle. Most patients experience a delay in diagnosis; this happens for a variety of reasons. Women may dismiss symptoms as mild or unimportant and delay seeking medical attention.
Alternatively, many physicians treat patients on the basis of their symptoms without performing a biopsy of the lesion. About 50% of vulvar cancer patients experience prolonged pruritis or have an ulcerated or palpable mass on their vulva.
Vulvar cancer is easily mistaken for other conditions.
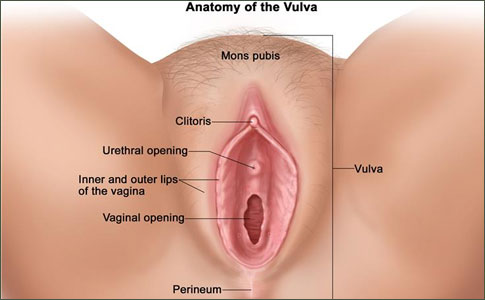
There is no absolute consistency in the appearance of vulvar lesions such as VIN, lichen sclerosis, or squamous cell hyperplasia that allows them to be easily distinguished from vulvar cancer. Therefore, it is best to advise that any suspicious areas should be biopsied. Examination of the vulva should include a thorough inspection of the perineal area, including areas around the clitoris and urethra. Palpation of the Bartholin's glands should be performed as well. Biopsies may be guided by use of toluidine blue dye (1%) or dilute acetic acid. Uptake of blue dye is increased in neoplastic cells with enlarged nuclei. This increased nuclear to cytoplasmic ratio is also responsible for the altered appearance of neoplastic cells treated with acetic acid (causing them to appear more white than surrounding tissues). Abnormally pigmented lesions suspicious for melanoma should be biopsied by a gynecologist or gynecologic oncologist familiar with the anatomy of the region because wide excisional margins are required.
More than 85% of vulvar malignancies are of squamous histology. About 5% of vulvar cancers are melanomas. Squamous cell cancer of the vulva is usually indolent, growing slowly and metastasizing late in its course. Local extension of the tumor occurs first, followed by lymphatic invasion. In general, lymphatic spread occurs in an organized, progressive fashion with superficial inguinal nodes affected before deeper (inguinofemoral and pelvic) nodal chains become involved.
Staging and therapy are primarily surgical, and the extent of resection is related to the stage of the tumor and the likelihood of nodal metastases.
For lesions with less than 1 mm of invasion, radical wide local excision will suffice. Stage I lesions (≤2 cm) can be treated effectively with modified radical hemivulvectomy and ipsilateral superficial inguinal node dissection (Figure 37.6). Larger tumors usually require radical vulvectomy and inguinal lymphadectomy (Figure 37.7). Larger tumors may also be treated primarily with radiotherapy and concurrent chemotherapy followed by surgical resection of residual disease. Pelvic exenteration is sometimes employed for women with extensive disease or as a salvage strategy for patients with recurrent cancer. Postoperative morbidity is related to the extent of the surgery. Therefore, the most conservative operation that can effectively treat the patient's condition is performed. As with the cancers previously discussed here, elderly patients with vulvar cancer should be allowed to receive the full benefit of optimal surgical therapy, as age alone is a poor determinant of surgical risk.
Types of vulvar cancer
Squamous cell carcinomas
Most cancers of the vulva are squamous cell carcinomas. This type of cancer begins in squamous cells, the main type of skin cells. There are several subtypes of squamous cell carcinoma:
The keratinizing type is most common, and usually develops in older women, and is not linked to infection with human papilloma virus (HPV).
Basaloid and warty types are less common, and are the kinds more often found in younger women with HPV infections.
Verrucous carcinoma is an uncommon subtype that is important to recognize because it is slow-growing and tends to have a good prognosis (outlook). This cancer looks like a large wart and a biopsy is needed to determine it is not a benign (non-cancerous) growth.
Adenocarcinoma
Cancer that begins in gland cells is called adenocarcinoma. About 8 of every 100 vulvar cancers are adenocarcinomas. Vulvar adenocarcinomas most often start in cells of the Bartholin glands. These glands are found just inside the opening of the vagina. A Bartholin gland cancer is easily mistaken for a cyst (accumulation of fluid in the gland), so a delay in accurate diagnosis is common. Most Bartholin gland cancers are adenocarcinomas. Adenocarcinomas can also form in the sweat glands of the vulvar skin.
Paget disease of the vulva is a condition in which adenocarcinoma cells are found in the top layer of the vulvar skin. Up to 25% of patients with vulvar Paget disease also have an invasive vulvar adenocarcinoma (in a Bartholin gland or sweat gland). In the remaining patients, the cancer cells are found only in the skin's top layer and have not grown into the tissues below.
Melanoma
Melanomas are cancers that develop from the pigment-producing cells that give skin color. They are much more common on sun-exposed areas of the skin, but can start in other areas, such as the vulva. Vulvar melanomas are rare, making up about 6 of every 100 vulvar cancers.
Sarcoma
A sarcoma is a cancer that begins in the cells of bones, muscles, or connective tissue. Less than 2 of every 100 vulvar cancers are sarcomas. Unlike other cancers of the vulva, vulvar sarcomas can occur in females at any age, including in childhood.
Basal cell carcinoma
Basal cell carcinoma, the most common type of skin cancer, is more often found on sun-exposed areas of the skin. It occurs very rarely on the vulva.
Survival is related to clinical stage and the extent of nodal involvement. Five-year survival for stages I and II vulvar cancer treated by standard surgical means is of the order of 90%. Survival (for all stages) still exceeds 70% in the absence of lymph node metastasis. However, lymphatic spread portends a worse outcome. Patients found to have inguinal lymph node metastases are usually treated with inguinal and pelvic radiation therapy postoperatively.
Vulvar cancer is a rare disease in which malignant (cancer) cells form in the tissues of the vulva.
Vulvar cancer forms in a woman's external genitalia. The vulva includes:
- Inner and outer lips of the vagina.
- Clitoris (sensitive tissue between the lips).
- Opening of the vagina and its glands.
- Mons pubis (the rounded area in front of the pubic bones that becomes covered with hair at puberty).
- Perineum (the area between the vulva and the anus).
Vulvar cancer most often affects the outer vaginal lips. Less often, cancer affects the inner vaginal lips, clitoris, or vaginal glands.
Vulvar cancer usually forms slowly over a number of years. Abnormal cells can grow on the surface of the vulvar skin for a long time. This condition is called vulvar intraepithelial neoplasia (VIN). Because it is possible for VIN to become vulvar cancer, it is very important to get treatment.
Signs of vulvar cancer include bleeding or itching.
Vulvar cancer often does not cause early signs or symptoms. Signs and symptoms may be caused by vulvar cancer or by other conditions. Check with your doctor if you have any of the following:
- A lump or growth on the vulva.
- Changes in the vulvar skin, such as color changes or growths that look like a wart or ulcer.
- Itching in the vulvar area, that does not go away.
- Bleeding not related to menstruation (periods).
- Tenderness in the vulvar area.
Gynecologic Cancers |
Only one-third of patients survive 5 years if nodal metastasis is present. Involvement of the deeper, pelvic nodes results in a 20% 5-year survival rate. Approximately 80% of recurrences occur in the first 2 years after treatment. The majority of recurrences occur near the site of the primary lesion. Seventy-five percent of patients with locally recurrent disease (limited to the vulva) can be salvaged with radical wide local excision. In contrast, patients who develop a groin recurrence are rarely curable, and palliative surgical resection is associated with a high risk of complications.
Most typical symptoms include:
- Dyspareunia - painful sexual intercourse
- Bleeding
- Burning
- Dark discoloration in cases of melanoma
- Dysuria - painful urination
- Persistent itching
- The area may be sensitive and raw
- Wart-like growths
What causes vulvar cancer?
Cancer is a class of diseases characterized by out-of-control cell growth. Cancer harms the body when damaged cells divide uncontrollably to form lumps or masses of tissue called tumors (except in the case of leukemia where cancer prohibits normal blood function by abnormal cell division in the blood stream). Tumors can grow and interfere with and alter body function. Tumors that stay in one spot and demonstrate limited growth are generally considered to be benign, dangerous cancer that spreads is malignant.
More dangerous, or malignant, tumors form when two things occur: 1. a cancerous cell manages to move throughout the body using the blood or lymph systems, destroying healthy tissue in a process called invasion. 2. that cell manages to divide and grow, making new blood vessels to feed itself in a process called angiogenesis.
If the patient with malignant cancer receives no treatment, it can grow and spread to other parts of the body (metastasis). As soon as the cancer gets into the lymphatic system it can more effectively reach other parts of the body, including vital organs.
Experts do not know exactly why the runaway growth of cancer cells starts. We do know, however, that certain risk factors increase the probability of developing the disease. These include:
- Human papilloma virus (HPV) - women infected with HPV have a higher risk of developing vulval cancer.
- Vulvar intraepithelial neoplasia (VIN) - this is a general term for a precancerous state in which certain cells within the vulvar epithelium have a range of low-grade carcinoma. Women with VIN have a significantly higher risk of developing vulval cancer.
- Sexually transmitted infections - women with antibodies to the herpes simplex virus type 2 have been linked to a higher increase of vulval cancer.
- Systemic lupus erythematosus- one study showed a three-fold increase in vulval cancer risk.
- Smoking- studies have revealed an association between regular smoking and vulval cancer, ranging from a three-fold to six-fold increase. If the regular smoker also has HPV infection, the risk is much higher still.
- Kidney transplant - women who have had a kidney transplant have a much higher risk of developing vulval cancer. Doctors believe it is due to the immunosuppressant drugs (to stop organ rejection by the body) the patient has to take for life.
- Human immunodeficiency virus (HIV)- People with HIV/AIDS are more susceptible to HPV infection.
- Psoriasis - women with psoriasis have a significantly higher risk of developing vulval cancer.
The most common complications of treatment are related to wound breakdown and infection and occur in approximately 15% of patients. Other complications that arise in the early postoperative period include urinary tract infection, hematomas, seromas, venous thromboembolic disorders, femoral nerve injury manifestations, and osteitis pubis. Late complications may include lymphangitis, stress urinary incontinence, lymphocyst formation, introital stenosis, vaginal fistula, femoral hernia, and sexual dysfunction, but the most common late complication is intractable leg edema (lymphedema).
Estrogen replacement can usually be given to these patients. Hormonal treatment may help to maintain the health of surrounding perineal and vaginal tissues postoperatively.
How is vulvar cancer diagnosed?
The doctor will carry out a gynecologic evaluation, which includes checking the vulva - this may reveal the presence of an ulceration, lump, or a mass. If a lesion looks suspicious a biopsy is required. The examination of the vulva should include the perineal area, including areas around the clitoris and urethra, as well as the Bartholin's glands (palpation). If necessary anesthesia can be used for a more thorough examination.
Depending on the results of the biopsy, the doctor may order further tests:
- Cystoscopy: The bladder is examined to determine whether the cancer has spread to that area.
- Proctoscopy: The rectum is examined to check whether the cancer has spread to the rectal wall.
- Imaging scans: Imaging scans can help the doctor determine whether the cancer has spread, and if so, where to. An MRI or CT scan may be used. X-rays may be used to determine whether the cancer has reached the lungs.
Staging of vulvar cancer
If a biopsy confirms the presence of vulval cancer, the doctor will stage it with the help of imaging (CT or MRI). Staging guidelines used in the UK:
- Stage 0 - known as carcinoma in situ; the cancer only exists on the surface of the skin.
- Stage 1 - the cancer is limited to the vulva or perineum and is up to 2cm in size.
- Stage 2 - same as 1, but the tumor is at least 2cm in size.
- Stage 3 - the cancer has reached nearby tissue, such as the anus or vagina. It may also have reached the lymph nodes.
- Stage 4 - the cancer has reached lymph nodes on both sides (of the groin). It may also have reached the urethra (where urine comes out of), the bowel or the bladder.