Health Centers > Sexual Health Center > Sexual and Gender Identity Disorders > Erectile Dysfunction
Erectile Dysfunction
Anatomy
The key structures mediating penile erection are the paired corpora cavernosa or 'erectile bodies' (Figure 1). These cylindrical structures form the bulk of the penis and fill with arterial blood under pressure at the time of erection. Fused distally for three- quarters of their length, they separate proximally to fuse with each ischial tuberosity of the pelvis.
A Review of Erectile Dysfunction
Arterial Blood Supply
Venous Drainage
Lymphatic Drainage
Neuroanatomy
Central Nervous System Connections
- Mechanisms of erection
- Causes of erectile dysfunction
Vasculogenic Causes
Neurogenic Causes
Endocrinological Causes
Priapism and Postpriapism ED
Psychogenic Causes
- Epidemiology of erectile dysfunction
- Risk factors for erectile dysfunction
- Diagnosis of erectile dysfunction
History
Physical Examination
Special Investigations
- Treatment of erectile dysfunction
Psychosexual Counseh5ng
Medical Therapies
Vacuum Decices
Surgical Therapies
- Erectile Dysfunction - Conclusions
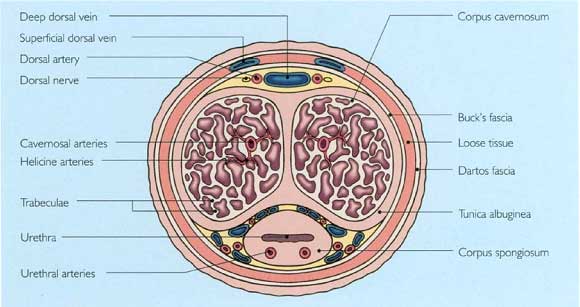
Each corpus cavernosum has a thick fibrous sheath, the so-called tunica albuginea, which surrounds the erectile tissue, made up of multiple lacunar spaces that are inter-connected and lined by vascular endothelium (Figure 2). The trabeculae constitute the walls of these spaces, and comprise smooth muscle and a fibroelastic framework of collagen in almost equal quantities.
The corpus spongiosum surrounds the urethra, which traverses the length of the penis within this structure, lying in the ventral groove formed by the paired corpora cavernosa in the pendulous portion. At its proximal portion, it expands to form the bulb, which curves upwards through the urogenital diaphragm to reach the apex of the prostate gland. Distally, the corpus spongiosum expands to form the glans penis (Figure 3). The spongiosum is composed of sinusoidal spaces of larger dimensions than those of the corpora cavernosa and with less smooth muscle. The tunica albuginea surrounding the spongiosum is flimsy compared with that of the corpora, but the spongiosum is nevertheless capable of an erectile response. 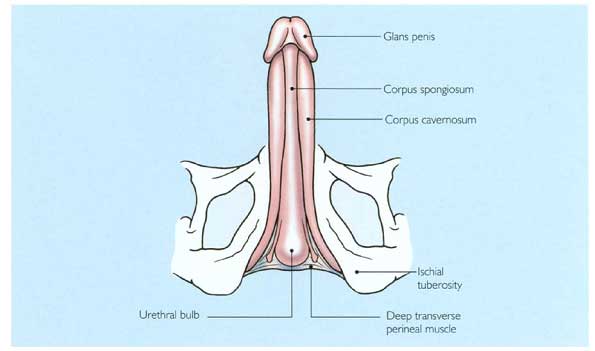
The corpus spongiosum in the bulbar region is surrounded by the bulbospongiosus muscles (Figure 4). These have two important functions: to facilitate ejaculation by their rhythmic contractions, and to empty the bulbar urethra after voiding, thereby preventing postmicturition dribble.
The skin overlying the penis is exceptionally mobile and expandable to accommodate the considerable increase in girth and length that occurs during erection. This lack of adherence makes it relatively susceptible to edema. In its distal portion, the penile skin extends forward to form the prepuce before folding backwards and attaching to the corona of the glans penis (Figure 5).
The pendulous portion of the penis is supported and stabilized by the suspensory ligament (Figure 6). Division of this structure makes the penis appear longer in its flaccid state, but this does not enhance the proportions of the organ when erect.
Male Infertility
Primary infertility affects 15-20% of married couples. Approximately one-third of cases ...
Arterial Blood Supply
The blood supply to each corpus cavernosum is derived mainly from the internal iliac artery, a branch of the atheroma-prone common iliac artery. In the pelvis, the internal pudendal artery passes beneath the sacrospinous ligament and over the sacrotuberous ligament, and gives off the perineal artery in Alcock's canal, where it runs under the superficial transverse perineal muscle and the symphysis pubis (Figure 7). After giving off the perineal artery, it becomes the common penile artery (Figure 8). This vessel pierces the pelvic floor adjacent to the inferior ramus of the ischium near the bulb of the urethra and gives off the bulbar, urethral, dorsal and cavernosal branches before reaching the corpus cavernosum to form one element of the paired dorsal arteries (Figure 8).
The cavernosal artery on each side pierces the tunica albuginea at the hilum of the penis. It then runs distally in the center of each corpus while giving off numerous helicine branches. These corkscrewshaped muscular vessels open directly into the lacunar spaces (Figure 9). The tonic contraction of the smooth muscle walls (Figure 10) normally allows only small amounts of blood into the lacunar spaces, thereby maintaining penile flaccidity. Relaxation of the muscular walls of these vessels initiates the hemodynamic changes that result in penile erection.
Venous Drainage
Blood leaves the penis via three venous systems: superficial, intermediate, and deep. The superficial system allows blood from multiple superficial veins to drain into the superficial dorsal vein, which itself drains into the left external branch of the internal saphenous vein. The intermediate venous system lies beneath Buck's fascia and comprises the deep dorsal vein and the multiple circumflex veins. This system drains blood from the glans, corpus spongiosum and the distal two-thirds of the corpora. The deep dorsal vein runs in the groove dorsally between the corpora cavernosa. It enters the pelvis beneath the suspensory ligament, which suspends the corpora from the undersurface of the pubic arch and drains into the dorsal venous complex at the urethroprostatic junction. The deep drainage system consists of the cavernosal and crural veins. Emissary veins in the proximal third of the penis join to form one or two cavernosal veins which pass between the bulb and crus of the penis to drain into the internal pudendal vein (Figure 11).
Lymphatic Drainage
Lymph is drained from the penis by lymphatics which pass to the superficial and deep inguinal lymph nodes of the femoral triangle (Figure 12). In turn, these nodes, which may become secondarily involved in patients who have carcinoma of the penis (Figure 13), drain to the external and internal iliac lymphatic chains. Conditions that obstruct these lymphatic channels, such as metastatic prostate cancer, may result in gross penile and scrotal edema.
Neuroanatomy
Three sets of peripheral nerves are involved in penile erection and subsequent detumescence: parasympathetic nerves from the second to fourth sacral (S2-S4) segments, sympathetic nerves from the tenth thoracic to the second lumbar (T10-L2) thoracolumbar outflow, and somatic fibers via the pudendal nerves (Figure 14).
The sympathetic nerves reach the corpora, as well as the prostate and bladder neck, via the hypogastric nerves, where they are susceptible to injury in retroperitoneal lymph node dissection performed for the treatment of metastatic testicular cancer.
Postganglionic noradrenergic fibers pass posterolateral to the prostate in the so-called nerves of Walsh to enter the corpora cavernosa medially.
Parasympathetic nerves stem from the so-called sacral erection center and their cell bodies lie in the intermediolateral nuclei from S2 to S4. Exiting through the sacral foramina, these nerves pass forward lateral to the rectum as the nervi erigentes to reach the pelvic plexus. In this location, preganglionic fibers relay in ganglia, and postganglionic non-adrenergic, non-cholinergic (NANC) fibers pass in the cavernous nerves to the corpora cavernosa. These nerves are vulnerable during procedures such as abdominoperineal resection of the rectum and radical prostatectomy (Figure 15).
The pudendal nerves comprise motor efferent and sensory afferent fibers which innervate the ischiocavernosus and bulbocavernosus muscles as well as the penile and perineal skin. Pudendal motor neuron cell bodies are located in Onuf's nucleus of the S2-S4 segments. The pudendal nerve enters the perineum through the lesser sciatic notch at the posterior border of the ischiorectal fossa and runs in Alcock's canal towards the posterior aspect of the perineal membrane. At this point, it gives off the perineal nerve with branches to the scrotum and the rectal nerve supplying the inferior rectal region.
The dorsal nerve of the penis emerges as the last branch of the pudendal nerve. It then runs distally along the dorsal penile shaft lateral to the dorsal artery. Multiple fascicles fan out distally, supplying proprioceptive and sensory nerve terminals to the dorsum of the tunica albuginea and skin of the penile shaft and glans penis.
Central Nervous System Connections
Although reflex spinal erections may occur provided that the sacral reflexes are intact (for example, after cervical or thoracic spinal injury), central connections are paramount in engendering the normal male sexual response. These central pathways, however, are as yet incompletely understood.
A number of areas in the brain are involved in the modulation of erection, including the thalamic nuclei, rhinencephalon, limbic structures and paraventricular nucleus. Messages are integrated in the medial preoptic area where dopaminergic neurons are important. Norepinephrine (noradrenaline) and serotonin have also been identified as neurotransmitters in this region. Efferent pathways enter the medial forebrain bundle and pass caudally into the mid-brain tegmental region near the lateral part of the substantia nigra. Caudal to the mid-brain, the efferent pathway travels in the ventrolateral part of the pons and medulla, passing down to the sacral spinal centers via the lateral funiculus of the spinal cord. Activation of the parasympathetic neurons, located in the spinal cord, leads to intrapenile release of nitric oxide, mainly by neural terminations.
Superimposed on this hypothalamo-spinal circuit are higher centers, including the gyrus rectus, cingulate gyrus and hippocampus; these areas are all capable of modifying the erectile response, although their exact function has not yet been elucidated. Diseases specifically affecting these structures include Parkinson's disease, multiple system atrophy and stroke, all of which are often associated with erectile dysfunction.









