Lung Cancer: Who is a Candidate for Surgery?
PATIENT SUITABILITY
The incidence of complications after lung resection is 2-5% for otherwise healthy patients and increases up to 50% in those with lung disease (3). The majority of patients with lung cancer are older and have a history of smoking with chronic obstructive pulmonary or heart disease. Patients with cardiac symptoms should undergo further evaluation such as stress testing. While the surgical mortality ranges from 4-12%, cardiac and pulmonary complications occur in up to 30% of patients (8). Once a patient is determined to be a candidate for curative resection by appropriate staging, the patient’s functional capacity is evaluated to predict the possibility of perioperative complications, long-term respiratory failure, or death. Factors such as the extent of proposed resection, preoperative lung function, and other medical problems are considered. Age by itself is not a major risk factor (3).
Pulmonary Function
While healthy adults have a large pulmonary reserve, most patients with lung cancer have decreased lung function due to a history of smoking. One of the goals of preoperative evaluation is to avoid severe postoperative respiratory insufficiency after lung resection while identifying the maximum number of patients who would tolerate pulmonary resection since it remains the only curative therapy available. All patients undergoing lung resection should have pulmonary function testing. The forced expiratory volume in one second (FEV1) and the predicted postoperative FEV1 are the parameters most commonly used and have the highest predictive value with lower volumes associated with an increased risk. Pulmonary function tests are sensitive, but not specific, and are useful in either approving patients for resection or identifying high-risk patients that require further evaluation.
Prior to performing lung resection in high-risk patients, it is crucial to determine the function of the remaining lung using tests such as quantitative ventilation and perfusion testing. After an intravenous injection and inhalation of technetium-labeled particles, the percentage of radioactivity distributed to each lung correlates with its contribution to lung function allowing a prediction of post-resection function. Resection of poorly functional lung may have relatively little effect on postoperative function. The predicted postoperative FEV1 has been correlated with the occurrence of postoperative respiratory complications. Exercise testing, including stair climbing, treadmill tests, and bicycle ergometry, is also useful and stresses the entire cardiopulmonary system of oxygen delivery. Measuring the maximum oxygen uptake during exercise testing may also be useful in predicting postoperative complication rates, particularly for patients with other testing indicating limited pulmonary reserve. . Proper patient selection using such techniques has been correlated with decreases in complication rates, time on mechanical ventilation, and length of hospital stay (9).
We have adopted an algorithm for the preoperative functional assessment for lung resection shown in Figure 6. However, due to the poor prognosis of NSCLC managed non-operatively, all patients should be considered for resection, and the final decision on whether to proceed depends on multiple factors with each patient considered individually.
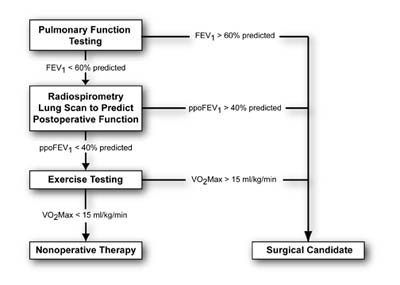 Figure 6. Algorithm outlinkint the preoperative functional evaluation for lung cancer resection. (FEV1, forced expiratory volume in one second; ppo, predicted postoperive: VO2Max, oxygen uptake)
Figure 6. Algorithm outlinkint the preoperative functional evaluation for lung cancer resection. (FEV1, forced expiratory volume in one second; ppo, predicted postoperive: VO2Max, oxygen uptake)
Risk Factor Modification
Potentially modifiable risk factors include symptomatic obstructive airway disease, smoking, obesity, and malnutrition. Aggressive pre- and perioperative management can decrease pulmonary complications by 50%. Long-term smoking is the most important risk factor for lung carcinoma, and a smoking history greater than 20 pack years significantly increases the surgical risks (10). Smoking cessation more than eight weeks prior to coronary artery bypass decreased the risk of pulmonary complications to that of nonsmokers (11). Preoperative teaching, optimization of medications for obstructive pulmonary disease, and an exercise program may also be important in minimizing postoperative complications.