Thyroid Cancer Treatment Varies by Hospital
Where thyroid cancer patients go for care plays a large role in whether they receive radioactive iodine treatment, a new study from the University of Michigan Comprehensive Cancer Center finds.
While the size and severity of the tumor also played a role in treatment, researchers found unexplained hospital factors had a significant impact on radioactive iodine use.
“What hospital you go to makes a difference in use of radioactive iodine. It doesn’t just matter what the tumor looks like, but where you go for care,” says lead study author Megan Haymart, M.D., assistant professor of internal medicine at the U-M Medical School.
Results of the study appear in the Aug. 17 issue of the Journal of the American Medical Association.
Thyroid cancer is currently one of the 10 most common cancers in the United States and is expected to become even more common in the next decade as more small, early stage cancers are uncovered.
Radioactive iodine following surgery to remove the thyroid is known to be an effective treatment for advanced or high-risk thyroid cancer that is very likely to return. But patients with small, low-risk disease often have an excellent prognosis without radioactive iodine treatment, giving some doctors pause to wonder whether they are submitting patients to unnecessary treatment and risk of side effects.
 “For some patients, radioactive iodine is a very important part of treatment, but for others, the risks may outweigh the benefit. We need more studies of this low-risk group of patients to understand what the best treatment course is,” Haymart says.
“For some patients, radioactive iodine is a very important part of treatment, but for others, the risks may outweigh the benefit. We need more studies of this low-risk group of patients to understand what the best treatment course is,” Haymart says.
In the current study, researchers looked at data from 189,219 patients diagnosed with thyroid cancer between 1990 and 2008, as reported to the National Cancer Database, a national database that captures about 85 percent of all thyroid cancers diagnosed in the United States.
Researchers found that radioactive iodine treatment is being used more frequently overall – 40 percent of patients in 1990, compared to 56 percent of patients in 2008. Size and severity of the tumor did impact a patient’s likelihood to have radioactive iodine, accounting for about 21 percent of the variation in care. In addition, factors such as whether the hospital saw a high volume of thyroid cancer patients played a role. But 29 percent of the variation between whether patients received radioactive iodine was attributable to hospital factors that could not be explained.
 “Even among people who are high risk – and the guidelines are clear that these patients should receive radioactive iodine – there is still variation. This suggests doctors are unclear about the indications for radioactive iodine. We need randomized clinical trials that look at radioactive iodine in low-risk patients so that we can set better guidelines for its use,” Haymart says.
“Even among people who are high risk – and the guidelines are clear that these patients should receive radioactive iodine – there is still variation. This suggests doctors are unclear about the indications for radioactive iodine. We need randomized clinical trials that look at radioactive iodine in low-risk patients so that we can set better guidelines for its use,” Haymart says.
Radioactive iodine treatment can have long-term side effects, including risk of a second cancer or damage to nearby tissue such as salivary glands. In addition, safety precautions need to be taken when the treatment is delivered, requiring patients to stay away from young children for a week and avoid becoming pregnant for up to a year after treatment.
Thyroid cancer statistics: 44,670 Americans will be diagnosed with thyroid cancer this year and 1,690 will die from the disease, according to the American Cancer Society
Additional authors: Mousumi Banerjee, Ph.D.; Ronald J. Koenig, M.D., Ph.D.; John D. Birkmeyer, M.D.; Jennifer J. Griggs, M.D., M.P.H., from U-M; and Andrew K. Stewart, M.A., from the American College of Surgeons
Funding: National Institutes of Health
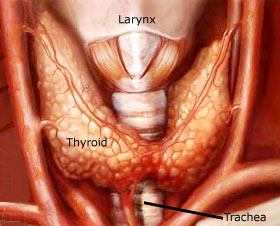
Different types
The types of thyroid cancer are:
- Papillary carcinoma - the most common form of thyroid cancer, which accounts for 70 to 80 per cent of cases. This cancer affects the cells that produce thyroid hormone. It grows slowly.
- Follicular carcinoma - this cancer also affects thyroid hormone-producing cells. However, it grows more quickly. This cancer accounts for around 10 per cent of thyroid cancers.
- Medullary carcinoma - this type of cancer tends to run in families. The symptoms may mimic those of Cushing’s syndrome. It does not involve thyroid hormone-producing cells and accounts for 5 to 10 per cent of thyroid cancers.
- Anaplastic carcinoma - this is the most aggressive and malignant form of thyroid cancer. It tends to grow rapidly and block the windpipe. It generally originates in benign or low grade cancerous thyroid tumours and accounts for around 7 per cent of thyroid cancers.
- Thyroid lymphoma - this occurs when white blood cells (lymphocytes) invade the thyroid and become cancerous. This accounts for around 4 per cent of thyroid cancers.
Risk factors
Anyone can develop thyroid cancer, regardless of age or gender. Some of the risk factors associated with thyroid cancer include:
- Radiation exposure - high doses of radiation were used during the 1950s to treat disorders of the throat and skin. Absorbed radioactive fallout following nuclear accidents is also a risk factor.
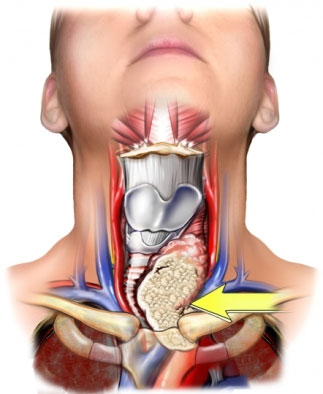
- Chronic goitre –persistent enlargement of the thyroid gland.
- Family history - a susceptibility can be inherited.
- Gender - more women than men develop thyroid cancer.
Disclosure: None
Reference: Journal of the American Medical Association, Vol. 306, No. 7, Aug. 17, 2011. “Use of Radioactive Iodine for Thyroid Cancer”
Resources:
U-M Cancer AnswerLine, 800-865-1125
###
Source: University of Michigan Health System