A new view of brain tumors
In the battle against brain cancer, doctors now have a new weapon - a new imaging technology that will make brain surgery dramatically more accurate by allowing surgeons to distinguish - at a microscopic level - between brain tissue and tumors.
Called SRS microscopy - short for stimulated Raman scattering - a team of researchers that included Xiaoliang Sunney Xie, the Mallinckrodt Professor of Chemistry and Chemical Biology and Minbiao Ji, a Post-Doctoral Fellow in Chemistry and Chemical Biology, were able to “see” the tiniest areas of tumor cells in brain tissue, and to distinguish tumor from healthy tissue in the brains of living mice - and then showed that the same was possible in tissue removed from a patient with glioblastoma multiforme, one of the most deadly brain tumors. The research is described in a September 4 paper in Science Translational Medicine.
“Biopsy has been the gold standard for detecting and removing these types of tumors,” said Xiaoliang Sunney Xie, the Mallinckrodt Professor of Chemistry and Chemical Biology and co-lead author of the paper. “But this technique, we believe, is better because it’s live. Surgeons can now skip all the steps of taking a biopsy, freezing and staining the tissue - this technique allows them to do it all in vivo.”
Developed by Xie and colleagues in 2008, SRS works by shining non-invasive lasers into tissue and detecting the weak signal that emerges. By analyzing the signal’s spectrum, researchers can build images of the cellular makeup of the tissue.
By amplifying those signals, they were able to transform a technique that once took hours or days into one that works in real-time, and could offer a critical insight to surgeons in the operating room.
Since brain tissue and tumors contain different chemical makeups, researchers can create images that precisely show where tumor “margin” - the boundary area where tumor cells infiltrate among normal cells - is located, helping to guide surgeons in the operating room.
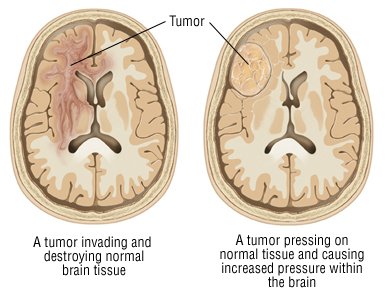 “It’s very nerve-wracking,” Xie said, of the challenge facing surgeons. “They have an MRI image, and they know what needs to be removed, but the question is where do you stop? A very experienced surgeon may be able to discern between brain tissue and a tumor based on subtle color differences, but many surgeons, I believe, will find this technology a useful guide.”
“It’s very nerve-wracking,” Xie said, of the challenge facing surgeons. “They have an MRI image, and they know what needs to be removed, but the question is where do you stop? A very experienced surgeon may be able to discern between brain tissue and a tumor based on subtle color differences, but many surgeons, I believe, will find this technology a useful guide.”
Working with a team of researchers led by Daniel Orringer, M.D., a lecturer in the U-M Department of Neurosurgery, Harvard researchers were able to show that the technique can be used to detect tumors in living mice, and in human brain tissue.
On average, Orringer said, patients diagnosed with glioblastoma multiforme live only 18 months after diagnosis. Surgery is among the most effective treatments for such tumors, but less than a quarter of patients’ operations achieve the best possible results, according to a study published last fall in the Journal of Neurosurgery.
“Though brain tumor surgery has advanced in many ways, survival for many patients is still poor, in part because surgeons can’t be sure that they’ve removed all tumor tissue before the operation is over,” said Orringer. “We need better tools for visualizing tumor during surgery, and SRS microscopy is highly promising. With SRS we can see something that’s invisible through conventional surgical microscopy.”
The authors suggest that SRS microscopy may be as accurate as Hematoxylin and eosin (H&E) staining - the current approach used in brain tumor diagnosis.
In one test described in the paper, H&E staining was pitted directly against SRS microscopy. Three surgical pathologists, trained in studying brain tissue and spotting tumor cells, had virtually the same level of accuracy, regardless of which images they examined. The difference, Xie said, is that SRS microscopy can be done in real time, and without dyeing, removing or processing the tissue.
“For more than 100 years, Hematoxylin and eosin stain has been the gold standard for this type of imaging,” Xie said. “But with this technology, we don’t need to freeze the tissue, we don’t need to stain tissue, and we don’t need to biopsy - this acts like an optical biopsy, and allows us to identify the tumor margins at a cellular level.”
“We are glad that this technology is now taking a step forward into a clinical application,” he added. “With this paper, we now have the proof of principle that this can be done in human brains in situ.”
###
Peter Reuell
.(JavaScript must be enabled to view this email address)
617-496-8070
Harvard University