Chemotherapy and stereotactic ablative radiation (SABR) consecutively may be promising treatment option for patients with advanced pancreatic cancer
For patients with locally advanced pancreatic cancer, the combination of chemotherapy and stereotactic ablative radiation (SABR) may be a promising treatment option, ultimately allowing them to undergo surgery that may not otherwise be an option, according to research presented today at the American Society for Radiation Oncology’s (ASTRO’s) 56th Annual Meeting.
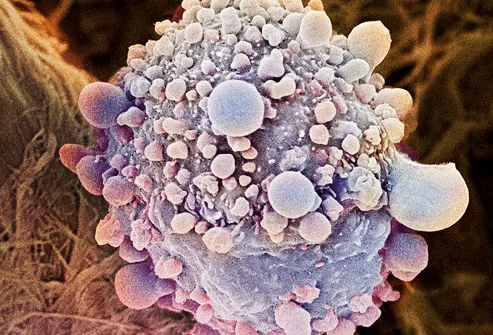
Surgery is the only potentially curative therapy for individuals with pancreatic ductal adenocarcinoma (PDA), the most common type of pancreatic cancer.
However, pancreatic cancer is often diagnosed at an advanced stage, making surgical removal of the tumor or the organ challenging, if not impossible. In addition, many patients with locally-advanced pancreatic cancer may have microscopic spread of the disease to other parts of the body.
Currently, there is no standard of care for treating patients with pancreatic cancer for whom surgery is not an option. Chemotherapy plays an important role in addressing microscopic disease. Stereotactic ablative radiation (SABR), with its shorter treatment times and precision that lowers the risk of damage to normal cells, is a promising treatment modality for patients with locally advanced PDA.
This prospective, single-arm, phase II clinical trial was conducted to evaluate the safety, feasibility, and efficacy of induction chemotherapy followed by SABR in 34 patients who had biopsy-proven PDA. Eighteen patients had borderline resectable PDA (the cancer was primarily located within the pancreas), and 16 patients had locally advanced PDA (the cancer had spread into nearby blood vessels). The average patient age was 71, and 56 percent of the patients were women.
Induction chemotherapy, consisting of gemcitabine and capecitabine, was administered over four, 21-day cycles to 31 of the 34 (91 percent) of the patients. Three of the patients did not complete chemotherapy - one died after consent but prior to chemotherapy; one died during chemotherapy because of an arterial occlusion; and one had a myocardial infarction prior to completion of the four courses of chemotherapy.
As evidenced by CT scan, the cancer did not grow or spread in all 31 patients who completed chemotherapy, thus all patients received three SABR treatments of 36 Gy each, including a 2mm expansion around the gross tumor. Four weeks following SABR, radiation oncologists, surgical oncologists and medical oncologists made a multidisciplinary decision as to whether each patient’s tumor could then be surgically removed.
 Of the 31 patients, 12 (40 percent) proceeded to pancreaticoduodenectomy (commonly referred to as “the Whipple procedure,” which removes the head of the pancreas, part of the small intestine, the gallbladder, the end of the common bile duct and sometimes a portion of the stomach). Ninety percent of patients who had surgery (11) had no local disease after surgery.
Of the 31 patients, 12 (40 percent) proceeded to pancreaticoduodenectomy (commonly referred to as “the Whipple procedure,” which removes the head of the pancreas, part of the small intestine, the gallbladder, the end of the common bile duct and sometimes a portion of the stomach). Ninety percent of patients who had surgery (11) had no local disease after surgery.
Ultimately, for this patient population, the findings translate to approximately 90 percent chance of local disease control at 1 year, and >20 months free of any disease recurrence.
“This is a promising treatment option that may prove not only to be more effective than chemotherapy alone prior to surgery, it may also be better than chemotherapy and standard radiation,” said lead study author Kimmen Quan, MD, a radiation oncologist at the University of Pittsburgh Medical Center. “Patients tolerated the chemotherapy and SABR regimen quite well, with excellent quality of life during treatment. These results appear to translate into better control of disease in the pancreatic region and a longer freedom from disease recurrence. This combination should be considered for patients with advanced pancreatic cancer, which is still treatable disease, and could potentially improve survival in this patient population.”
The abstract, “Interim Analysis of a Phase II Clinical Trial of Induction Gemcitabine/Capecitabine followed by SABR in Borderline/Locally Advanced Pancreatic Adenocarcinoma,” will be presented in detail during a scientific session at ASTRO’s 56th Annual Meeting at 4:15 p.m. Pacific time on Monday, September 15, 2014. To speak with Dr. Quan, please call Michelle Kirkwood on September 14 – 17, 2014, in the ASTRO Press Office at the Moscone Center in San Francisco at or 415-978-3503 or 415-978-3504, or email Michelle Kirkwood.
ASTRO’s 56th Annual Meeting, to be held at the Moscone Center in San Francisco, September 14-17, 2014, is the nation’s premier scientific meeting in radiation oncology. The 2014 Annual Meeting is expected to attract more than 11,000 attendees including oncologists from all disciplines, medical physicists, dosimetrists, radiation therapists, radiation oncology nurses and nurse practitioners, biologists, physician assistants, practice administrators, industry representatives and other health care professionals from around the world. Led by ASTRO President Bruce G. Haffty, MD, FASTRO, a radiation oncologist specializing in breast cancer, the theme of the 2014 Meeting is “Targeting Cancer: Technology and Biology,” and the Presidential Symposium, “Local-regional Management of Breast Cancer: A Changing Paradigm,” will feature Jay R. Harris, MD, FASTRO, and Thomas A. Buchholz, MD, FASTRO, to highlight recent practice-changing, landmark studies and current developments in the local-regional management of breast cancer. ASTRO’s four-day scientific meeting includes presentation of up to four plenary papers, 360 oral presentations, 1,862 posters and 144 digital posters in more than 50 educational sessions and scientific panels for 20 disease-site tracks. Three keynote speakers will address a range of topics including oncologic imaging, biology and targeting in oncology, and human error and safety concerns: Hedvig Hricak, MD, PhD, Chair of the Department of Radiology and the Carroll and Milton Petrie Chair at Memorial Sloan Kettering Cancer Center; Frank McCormick, PhD, FRS, DSc (hon), Professor Emeritus and the David A. Wood Distinguished Professor of Tumor Biology and Cancer Research of the University of California at San Francisco Helen Diller Family Comprehensive Cancer Center; and Sidney Dekker, PhD, MA, MSc, Professor and Director of the Safety Science Innovation Lab at Griffith University, Brisbane, Australia.
About ASTRO
ASTRO is the premier radiation oncology society in the world, with more than 10,000 members who are physicians, nurses, biologists, physicists, radiation therapists, dosimetrists and other health care professionals that specialize in treating patients with radiation therapies. As the leading organization in radiation oncology, the Society is dedicated to improving patient care through professional education and training, support for clinical practice and health policy standards, advancement of science and research, and advocacy. ASTRO publishes two medical journals, International Journal of Radiation Oncology -Biology - Physics (http://www.redjournal.org) and Practical Radiation Oncology (http://www.practicalradonc.org); developed and maintains an extensive patient website, http://www.rtanswers.org; and created the Radiation Oncology Institute (http://www.roinstitute.org), a non-profit foundation to support research and education efforts around the world that enhance and confirm the critical role of radiation therapy in improving cancer treatment.
###
American Society for Radiation Oncology