Biomarker identification may lead to new noninvasive test for colorectal cancer detection
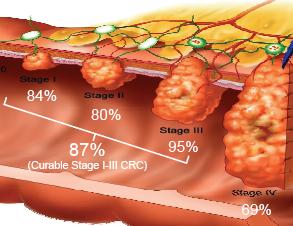
The average 5-year survival for colorectal cancer (CRC) is less than 10% if metastasis occurs, but can reach 90% if detected early. A new non-invasive test has been developed that measures methylation of the SDC2 gene in tissues and blood sera. This test detected 87% of all stages of colorectal cancer cases (sensitivity) without significant difference between early and advanced stages, while correctly identifying 95% of disease-free patients (specificity). The results are published in the July issue of The Journal of Molecular Diagnostics.
According to the US Centers for Disease Control and Prevention, CRC is the second leading cancer killer in the US affecting both men and women. In 2009, close to 137,000 people in the US were diagnosed with CRC, with close to a 40% mortality rate.
There are other screening choices for CRC, including fecal occult blood testing (FOBT), fecal immunochemical testing, and colonoscopy. Colonoscopy is the gold standard of CRC screening, but patient resistance - mostly due to the unpleasant preparation - has curbed widespread adoption. FOBT is non-invasive but has limited sensitivity, particularly for early disease. A sensitive and specific non-invasive test using blood or stool could to be a more preferable option with the potential of saving many lives.
In their search for a biomarker that could be used for the early detection of CRC, investigators from Genomictree, Inc. and Yonsei University College of Medicine in Seoul, South Korea, performed DNA microarray analysis coupled with enriched methylated DNA using tissues from primary tumors and non-tumor tissues from 12 CRC patients.
After step-wise filtering, they found a set of genes that were highly methylated across all of the CRC tumors. Ultimately they identified one gene, SDC2, which encodes the membrane syndecan-2 protein, a protein that is known to participate in cell proliferation, cell migration, and is expressed in colon mesenchymal cells. The methylation level of target region of SDC2 assessed in tumor tissue was found to be significantly higher than that from paired adjacent non-tumor tissue.
The next step was to clinically validate the biomarker by analyzing SDC2 methylation levels in primary tumors and paired-adjacent non-tumor tissue samples from 133 CRC patients. Investigators found that in the transcriptional regulatory region of the SDC2 gene, tumor samples showed significantly higher levels of methylation than the control samples. SDC2 methylation positivity ranged from 92.9% to 100% when samples were stratified according to stages of cancer.
 Further, investigators found that the SDC2 biomarker could be measured in serum samples from CRC patients and healthy individuals. “The SDC2 methylation test was able to detect 92% for detection of stage I cancer patients indicating that SDC2 is suitable for early detection of CRC where therapeutic interventions have the greatest likelihood of curing the patient from the disease,” says first author TaeJeong Oh, PhD.
Further, investigators found that the SDC2 biomarker could be measured in serum samples from CRC patients and healthy individuals. “The SDC2 methylation test was able to detect 92% for detection of stage I cancer patients indicating that SDC2 is suitable for early detection of CRC where therapeutic interventions have the greatest likelihood of curing the patient from the disease,” says first author TaeJeong Oh, PhD.
Abnormal growths in the colon or rectum
Most colorectal cancers develop slowly over several years. Before a cancer develops, a growth of tissue or tumor usually begins as a non-cancerous polyp on the inner lining of the colon or rectum.
A tumor is abnormal tissue and can be benign (not cancer) or malignant (cancer). A polyp is a benign, non-cancerous tumor. Some polyps can change into cancer, but not all do. The chance of changing into a cancer depends upon the kind of polyp:
- Adenomatous polyps (adenomas) are polyps that have the potential to change into cancer.
Because of this, adenomas are called a pre-cancerou s condition.
- Hyperplastic polyps and inflammatory polyps, in general, are not pre-cancerous. But some doctors think that some hyperplastic polyps can become pre-cancerous or might be a sign of having a greater risk of developing adenomas and cancer, particularly when these polyps grow in the ascending colon.
Another kind of pre-cancerous condition is called dysplasia. Dysplasia is an area in the lining of the colon or rectum where the cells look abnormal (but not like true cancer cells) whe n seen under a microscope. These cells can change into cancer over time. Dysplasia is usually seen in people who have had diseases such as ulcerative colitis or Crohn’s disease for many years. Both ulcerative colitis and Crohn’s disease cause chronic inflammation of the colon.
 The authors suggest that the SDC2 methylation test they describe could possibly be used as an alternative to or in conjunction with colonoscopy. It could also be used to monitor cancer progression and treatment. Dr. Sungwhan An, corresponding author and CEO of Genomictree, Inc., commented: “We are very excited with this result using a small amount of serum DNA from less than 1ml of blood. I believe a greater volume of blood will further improve the clinical performance of this test. We are currently preparing another set of clinical validation studies evaluating SDC2 methylation in serum DNA from patients with early adenoma.” In future research the authors will explore whether this biomarker is specific to CRC or universal among other cancers.
The authors suggest that the SDC2 methylation test they describe could possibly be used as an alternative to or in conjunction with colonoscopy. It could also be used to monitor cancer progression and treatment. Dr. Sungwhan An, corresponding author and CEO of Genomictree, Inc., commented: “We are very excited with this result using a small amount of serum DNA from less than 1ml of blood. I believe a greater volume of blood will further improve the clinical performance of this test. We are currently preparing another set of clinical validation studies evaluating SDC2 methylation in serum DNA from patients with early adenoma.” In future research the authors will explore whether this biomarker is specific to CRC or universal among other cancers.
Sigmoidoscopy - Sigmoidoscopy allows a physician to directly view the lining of the rectum and the lower part of the colon (the descending colon). This area accounts for about one-half of the total area of the rectum and colon.
Procedure - Sigmoidoscopy requires that you prepare by cleaning out the lower bowel. This usually involves consuming a clear liquid diet and using an enema shortly before the examination. Most people do not need sedative drugs and are able to return to work or other activities the same day. During the procedure, a thin, lighted tube is advanced into the rectum and through the left side of the colon to check for polyps and cancer; the procedure may cause mild cramping. Biopsies (small samples of tissue) can be taken during sigmoidoscopy. Sigmoidoscopy may be performed in a doctor’s office.
Effectiveness - Sigmoidoscopy can identify polyps and cancers in the descending colon and rectum with a high degree of accuracy. Studies have shown that sigmoidoscopy reduces the incidence of colorectal cancer and overall mortality.
Risks and disadvantages - The risks of sigmoidoscopy are small. The procedure creates a small tear in the intestinal wall in about 2 per every 10,000 people; death from this complication is rare. A major disadvantage of sigmoidoscopy is that it cannot detect polyps or cancers that are located in the right side of the colon.
Additional testing - Finding polyps or cancers in the lower colon increase the likelihood that there are polyps or cancer in the remaining part of the colon. Thus, if sigmoidoscopy reveals polyps or cancer, colonoscopy is recommended to view the entire length of the colon
###
David Sampson
.(JavaScript must be enabled to view this email address)
215-239-3171
Elsevier Health Sciences