Nanotech system, cellular heating may improve treatment of ovarian cancer
The combination of heat, chemotherapeutic drugs and an innovative delivery system based on nanotechnology may significantly improve the treatment of ovarian cancer while reducing side effects from toxic drugs, researchers at Oregon State University report in a new study.
The findings, so far done only in a laboratory setting, show that this one-two punch of mild hyperthermia and chemotherapy can kill 95 percent of ovarian cancer cells, and scientists say they expect to improve on those results in continued research.
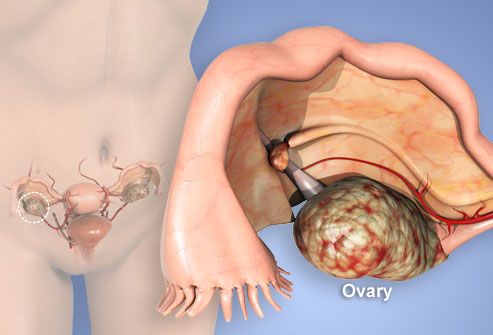
The work is important, they say, because ovarian cancer - one of the leading causes of cancer-related deaths in women - often develops resistance to chemotherapeutic drugs if it returns after an initial remission. It kills more than 150,000 women around the world every year.
“Ovarian cancer is rarely detected early, and because of that chemotherapy is often needed in addition to surgery,” said Oleh Taratula, an assistant professor in the OSU College of Pharmacy. “It’s essential for the chemotherapy to be as effective as possible the first time it’s used, and we believe this new approach should help with that.”
It’s known that elevated temperatures can help kill cancer cells, but heating just the cancer cells is problematic. The new system incorporates the use of iron oxide nanoparticles that can be coated with a cancer-killing drug and then heated once they are imbedded in the cancer cell.
Other features have also been developed to optimize the new system, in an unusual collaboration between engineers, material science experts and pharmaceutical researchers.
 A peptide is used that helps guide the nanoparticle specifically to cancer cells, and the nanoparticle is just the right size - neither too big nor too small – so the immune system will not reject it. A special polyethylene glycol coating further adds to the “stealth” effect of the nanoparticles and keeps them from clumping up. And the interaction between the cancer drug and a polymer on the nanoparticles gets weaker in the acidic environment of cancer cells, aiding release of the drug at the right place.
A peptide is used that helps guide the nanoparticle specifically to cancer cells, and the nanoparticle is just the right size - neither too big nor too small – so the immune system will not reject it. A special polyethylene glycol coating further adds to the “stealth” effect of the nanoparticles and keeps them from clumping up. And the interaction between the cancer drug and a polymer on the nanoparticles gets weaker in the acidic environment of cancer cells, aiding release of the drug at the right place.
“The hyperthermia, or heating of cells, is done by subjecting the magnetic nanoparticles to an oscillating, or alternating magnetic field,” said Pallavi Dhagat, an associate professor in the OSU School of Electrical Engineering and Computer Science, and co-author on the study. “The nanoparticles absorb energy from the oscillating field and heat up.”
The result, in laboratory tests with ovarian cancer cells, was that a modest dose of the chemotherapeutic drug, combined with heating the cells to about 104 degrees, killed almost all the cells and was far more effective than either the drug or heat treatment would have been by itself.
Doxorubicin, the cancer drug, by itself at the level used in these experiments would leave about 70 percent of the cancer cells alive. With the new approach, only 5 percent were still viable.
The work was published in the International Journal of Pharmaceutics, as a collaboration of researchers in the OSU College of Pharmacy, College of Engineering, and Ocean NanoTech of Springdale, Ark. It was supported by the Medical Research Foundation of Oregon, the PhRMA Foundation and the OSU College of Pharmacy.
“I’m very excited about this delivery system,” Taratula said. “Cancer is always difficult to treat, and this should allow us to use lower levels of the toxic chemotherapeutic drugs, minimize side effects and the development of drug resistance, and still improve the efficacy of the treatment. We’re not trying to kill the cell with heat, but using it to improve the function of the drug.”
Iron oxide particles had been used before in some medical treatments, researchers said, but not with the complete system developed at OSU. Animal tests, and ultimately human trials, will be necessary before the new system is available for use.
Drug delivery systems such as this may later be applied to other forms of cancer, such as prostate or pancreatic cancer, to help improve the efficacy of chemotherapy in those conditions, Taratula said.
###
David Stauth,
541-737-0787
SOURCE:
Oleh Taratula, 541-737-5785