Health Centers > Cancer Health Center > Cancer of the Oral Cavity
Cancer of the Oral Cavity
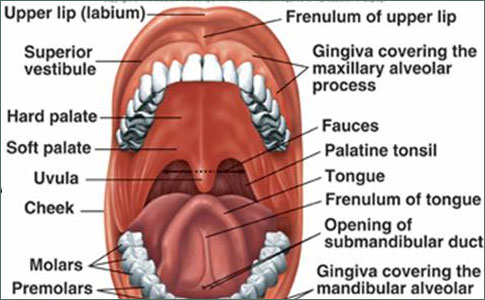
Anatomy
The vermilion border of the lips is the anterior boundary of the oral cavity, while the anterior tonsillar pillars, the posterior aspect of the hard palate, and the circumvallate papillae of the tongue are the posterior boundary. Subsites are (1) the vermilion surfaces of the lips; (2) the alveolar process of the mandible; (3) the alveolar process of the maxilla; (4) the retromolar trigone, which is the mucosa overlying the ascending ramus of the mandible behind the last lower molar tooth; (5) the hard palate; (6) the buccal mucosa, which lines the cheeks and inner aspects of the lips and includes the upper and lower buccoalveolar gutters; (7) the floor of the mouth; and (8) the anterior two-thirds of the tongue (oral tongue), which is limited posteriorly by the circumvallate papillae and includes the tip, dorsum, lateral borders, and undersurface of the oral tongue. The mucosa of the oral cavity consists of stratified squamous epithelium.
Cancer of the Oral Cavity
Anatomy
Pathology
Clinical Findings
Treatment
¬ Primary Cancer
¬ Management of Neck Metastases
Prognosis
References
Pathology
Over 95% of cancers of the oral cavity are squamous cell carcinomas. They are predominantly well and moderately well differentiated and can be preceded by premalignant lesions. Leukoplakia ("white patch") is induced by the same factors (tobacco, alcohol) that cause carcinomas. The malignant potential of leukoplakia corresponds to the degree of cellular dysplasia seen on biopsy. Erythroplakia ("red patch") usually shows severe cellular dysplasia and carries a 50% risk of malignant degeneration. Macroscopically, oral cancers can be exophytic growths, flat cancers with central ulceration and indurated edges, or deeply infiltrating ulcers. Verrucous carcinoma is an exophytic lesion that is histologically well differentiated and has a better prognosis than other oral cancers.
Oral cancers-especially those of the mucosa of the upper and lower alveolar ridges-often invade nearby bone. The mandible is most frequently involved. Minor salivary gland cancers arise in submucosal glands, which are most abundant in the hard palate. Ulceration is a late feature. Melanoma developing in the mucosa of the mouth is rare.
Cancers of the upper lip drain to parotid and submandibular nodes (level I), while those of the lower lip drain to submental and submandibular nodes (level I) and upper and mid jugular nodes (levels II and III). Midline cancers of the lip, the tongue, and the floor of the mouth can drain bilaterally. The incidence of cervical lymph node involvement from cancers of the oral cavity is related to the site and size of the primary cancer. Cancers of the oral tongue and the floor of the mouth have a higher incidence of cervical lymph node involvement than do cancers of the lip, hard palate, or buccal mucosa.
Anal Cancer: Strategies in Management
The management of anal cancer underwent an interesting transformation over the last two decades.
Clinical Findings
Patients with cancer of the oral cavity usually present with ulcerated cancers that have been present for weeks or months. They are typically men aged 50-70 years with a history of heavy tobacco and alcohol use. Dental hygiene is frequently poor, and areas of leukoplakia and erythroplakia can be seen adjacent to the cancer. Submandibular or jugular chain lymph nodes are palpable in 25-35% of patients. Pain is usually not a prominent feature but may become severe with deep infiltration.
T STAGE: ORAL CANCER
T1 Tumor 2 cm or less in greatest dimension T2 Tumor more than 2 cm but not more than 4 cm in greatest dimension T3 Tumor more than 4 cm in greatest dimension T4 Lip: Tumor invades adjacent structures (eg, through cortical bone, tongue, skin) T4 Oral cavity: Tumor invades adjacent structures (eg, through cortical bone, into deep [extrinsic] muscle of tongue, maxillary sinus, skin)
Treatment
A. Primary Cancer
Surgical excision is the treatment of choice for most oral cancers. Cancers of the vermilion surface of the lip are best treated with full-thickness excision of the lip. Lateral margins of 5 mm of uninvolved lip are taken with the cancer. The defect is closed primarily when one-third or less of the lip is excised. When excision of more than one-third of the lip is required, closure is achieved by transposition of a segment of the opposite lip on a vascular pedicle (Abbe flap). When the entire vermilion of the lip has been damaged, vermilionectomy (lip shave) can be performed along with excision of the cancer and a new vermilion surface created by advancing the labial mucosa.
Within the oral cavity, small cancers can usually be excised through the open mouth taking a margin of 1 cm of normal-appearing tissue. Small defects are closed by direct suture or split-thickness skin grafts. Larger cancers (> 2 cm) require more extensive exposure (ie, cheek flap), resection, and subsequent reconstruction. For cancers involving bone, marginal or segmental resection of the mandible is performed. A composite resection involves resection of an oral cancer, resection of a portion of the mandible, and a neck dissection.
Radiation therapy is an alternative to surgery for oral cancers smaller than 4 cm in diameter (T1 and T2 cancers). The side effects of mucositis, xerostomia, and osteoradionecrosis of the mandible must be balanced against potential advantages. T3 and T4 cancers are usually treated with combined surgery and radiation therapy to improve the rate of local control.
B. Management of Neck Metastases
Clinically apparent cervical lymph node metastases can be treated by radical neck dissection, which involves removal of all the lymphatic tissue of the neck along with the sternocleidomastoid muscle, internal jugular vein, and spinal accessory nerve. To save structures not directly involved by cancer, modified neck dissection is performed. A modified radical neck dissection always preserves the spinal accessory nerve, while a functional neck dissection always preserves the sternocleidomastoid muscle, the internal jugular vein, and the spinal accessory nerve. Selective neck dissections involve only certain cervical lymph node levels. For example, levels I, II, and III cervical lymph nodes and cervical lymph nodes in the upper portion of level V are removed with a supraomohyoid neck dissection while preserving the sternocleidomastoid muscle, the internal jugular vein, and the spinal accessory nerve.
When modified neck dissections are performed, adjuvant radiation therapy to the neck is frequently required. It is recommended for use when more than two cervical lymph nodes contain metastases, when more than one level of cervical lymph nodes are involved, or when there is extension of metastases through the capsule of a cervical lymph node. Occult cervical lymph node metastases are present in 20-30% of patients with oral cancers (other than lip, buccal mucosa, or hard palate cancers) who present with a clinically negative neck. Elective neck dissections have been advocated for these patients to more accurately stage the cancer and to prevent the need for a later and probably more radical neck dissection when the cervical lymph node metastases becomes clinically apparent. A supraomohyoid neck dissection is the dissection of choice in the elective situation.
Prognosis
The five-year survival rates for cancer of the oral cavity with appropriate treatment are as follows: stage I, 72-88%; stage II, 46-80%; stage III, 36-66%; and stage IV, 11-32%. Buccal mucosa cancers have a better prognosis than tongue or hard palate cancers.
Oral Cavity cancer -Natural History and Treatment by site
Both tumor and treatment significantly compromise speech and deglutition, particularly for those patients in whom cancer involves the tongue, the floor of the mouth, or the mandible. Furthermore, the diversity of potential sites of cancer development in the oral cavity and variations of lymphatic drainage and rates of node metastases lend added complexity to treatment planning. Despite the fact that this region is readily amenable to visual examination and bimanual palpation, more than 50% of patients are diagnosed in advanced stages » »
References
- Beenken S et al: T1 and T2 squamous cell carcinoma of the oral cavity: prognostic factors and the role of elective lymph node dissection. Head Neck 1999;21:124. Pubmed: 10091980
- Byers RM et al: Selective neck dissections for squamous carcinoma of the upper aerodigestive tract: patterns of regional failure. Head Neck 1999;21:499. Pubmed: 10449664
- Ferlito A et al: Changing concepts in the surgical management of the cervical node metastasis. Oral Oncol 2003;39:429. Pubmed: 12747966
- Matsuo JM et al: Clinical nodal stage is an independently significant predictor of distant failure in patients with squamous cell carcinoma of the larynx. Ann Surg 2003;238:412; discussion 421.
- Myers JN et al: Squamous cell carcinoma of the tongue in young adults: increased incidence and factors that predict treatment outcomes. Otolaryngol Head Neck Surg 2000;122:44. Pubmed: 10629481
- Samant S et al: Evaluation of neck dissection for improved functional outcome. World J Surg 2003;27:805. Pubmed: 14509511