Health Centers > Cancer Health Center > Benign Esophageal Tumors
Benign Esophageal Tumors
Benign Esophageal Tumors
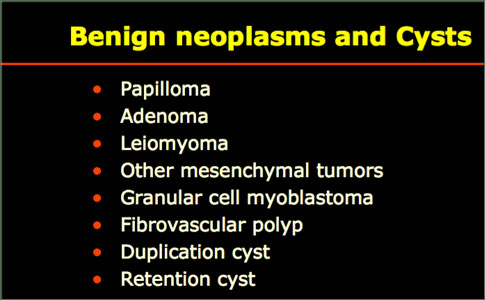
A variety of benign mass lesions can arise from different wall layers in the esophagus (Table 18-6). These tumors are usually asymptomatic and slow growing, noted only as incidental findings during routine radiography or endoscopy. Occasionally, they may be discovered during the evaluation of dysphagia or vague chest discomfort. The most common benign esophageal tumor is the leiomyoma. Because the tumor arises from the muscularis propria, it is covered by an intact submucosa and mucosa, making it difficult to biopsy endoscopically.
Benign Esophageal Tumors
Benign esophageal tumors
General Considerations
Clinical Findings
¬ Symptoms and Signs
¬ Imaging
Treatment
References
Inflammatory polyps and granulomas can arise in the setting of esophagitis and may be confused with malignant lesions from time to time. Endoscopic removal is possible, although usually not indicated. Endoscopic biopsy and regression with therapy for esophagitis clearly distinguish the clinical course of inflammatory polyps and granulomas from cancers.
Clinical Findings
Although the vast majority of benign esophageal tumors are clinically silent and go undetected, large or strategically located tumors may become symptomatic. Similar to their malignant counterparts, dysphagia is the most common presentation for patients with benign esophageal tumors. Less common presenting symptoms include odynophagia, retrosternal pain or thoracic pressure, food regurgitation, anorexia, and weight loss. Respiratory complaints such as cough, dyspnea, or sore throat may also contribute to the presentation. Occasionally, leiomyomas can outgrow their own blood supply, leading to necrosis and ulceration of the overlying mucosa and resulting in overt GI hemorrhage such as hematemesis or melena.
Many kinds of benign pathologic lesions occur in the esophagus. They include esophageal atresia, heterotopic gastric mucosa, heterotopic pancreatic tissue, diverticula, esophageal cyst, achalasia, Lye stricture, reflex esophagitis, Barrett's esophagus, herpes simplex esophagistis, cyto-megalovirus esophagitis, eosiphophilic esophagitis, Crohn's disease, candidiasis, leiomyoma, glycogenic acanthosis, amyloidosis, squamous papilloma, hyperplastic polyp, and granular cell tumor.
Recent advances in endoscopy have made it possible that these esophageal benign lesions are biopsied and diagnosed correctly. In the present study, the authors reviewed 931 archival cases of the esophageal biopsies in search for benign tumors of the esophagus.
Anal Cancer: Strategies in Management
The management of anal cancer underwent an interesting transformation over the last two decades.
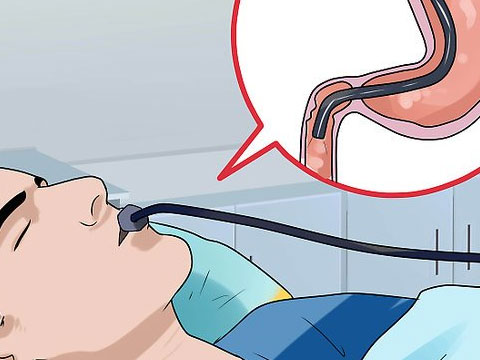
Endoscopic appearance and biopsy can identify some benign esophageal tumors. However, EUS provides high-resolution images that define the individual esophageal wall layers and can readily identify lesions in the deeper layers (ie, submucosa and muscularis propria) that elude endoscopic biopsy diagnosis.
If necessary, EUS-guided FNA can be performed for diagnostic purposes. Leiomyomas are generally noted as hypoechoic mass lesions within the muscularis propria. Occasionally, the echopattern is more heterogeneous, which may indicate hemorrhage into the tumor. Cystic lesions may appear as anechoic structures within the mucosa and submucosa, whereas inflammatory growths are always superficial and localized to the mucosa.
Treatment
Benign tumours of the oesophagus
Benign tumours of the oesophagus account for less than 1% of all oesophageal neoplasms. Leiomyomas are the most common; rarer entities include papillomas, fibrovascular polyps, granular cell tumours, adenomas, haemangiomas, neurofibromas, and lipomas.
Leiomyomas are smooth-muscle tumours arising in the oesophageal wall. They are usually solitary, well encapsulated with an intact overlying mucosa, and grow slowly. Most small (>5 cm) leiomyomas are asymptomatic and are incidental finding on barium study (see Barium contrast study showing the typical features of a leiomyoma of the oesophagus with a smooth semilunar defect in the contour of the oesophageal lumen and an intact mucosa, clear borders and a sharp angle between the tumour and the normal wall.). Diagnosis is made from the typical appearance on imaging, and endoscopy reveals intact mucosa. Sometimes leiomyomas can grow as an annular lesion producing dysphagia. There is no good evidence that they undergo malignant transformation to leiomyosarcoma.
Small, asymptomatic leiomyomas can be observed. Surgical removal is warranted for symptomatic or large leiomyomas (<5 cm). Simple enucleation is performed. Oesophageal resection is occasionally necessary for large or annular tumours.
Benign tumors of the esophagus are rare, and most of them are not clinically important lesions. However, differential diagnosis is important. In addition, large benign tumors may obstruct the esophageal lumen, and treatment was difficult in such cases. Squamous papilloma of the esophagus is a rare lesion.
Most of the previously reported study was case reports and studies of small series. The squamous papilloma of the esophagus does not transform into squamous cell carcinoma.
Granular cell tumor of the esophagus is extremely rare.
Only several case reports or studies of small series have been published. Its important point is differential diagnosis. In general, acidophilic granular cytoplasm and immunoreactions for vimentin, S100 protein, and neuron-specific enolase are important points in this tumor. The present 4 cases fulfilled the diagnostic criteria of granular cell tumor.
The frequency in the present study was 0.4%.
Tubular adenoma of the esophagus is extremely rare.
Only a few case reports are present in the literature. In the present study, it is very interesting that the tubular adenoma was associated with heterotopic gastric mcuosa.
Adenocarcinoma very infrequently develops in the heterotopic gastric mucosa. However, adenoma developing in heterotopic gastric mucosa has not been reported, to the author's best knowledge. In the present study, it frequency was 0.1%.
###
Gastroenterology Research - 2009;2:100-103
Esophageal cancer
Demographics & Epidemiology
Etiology
Natural History
¬ Clinical Presentation
¬ Complications
¬ Prognostic Factors
Diagnosis
Staging Techniques
Differential Diagnosis
Treatment
Surgery
¬ General Considerations
¬ Surgical Approach
Palliation Therapy
¬ Radiation Therapy
¬ Chemotherapy
¬ ¬ Single agent
¬ ¬ Combination chemotherapy
¬ ¬ Combined-modality therapy
¬ Endoscopic Therapy
¬ ¬ Dilation
¬ ¬ Ablation
¬ ¬ Photodynamic therapy (PDT)
¬ ¬ Endoscopic mucosal resection (EMR)
¬ ¬ Esophageal prostheses
Prognosis
Symptoms of Esophageal Submucosal Lesions
Esophageal submucosal lesions may not cause any symptoms. They are most often discovered during routine upper endoscopic examination of the esophagus for another problem, such as reflux disease (heartburn), abdominal pain, or unexplained weight loss. In some cases, these lesions can result in difficulty swallowing (dysphagia), food getting stuck in the esophagus, chest pain, or regurgitation of food. Some of these symptoms may ultimately cause weight loss.
Diagnosis of Esophageal Submucosal Lesions
Esophageal submucosal lesions are usually diagnosed incidentally by imaging methods such as computed tomography (CT), magnetic resonance imaging (MRI), or standard upper endoscopy. They appear as a "bulge" on an imaging test.
In order to better determine which type of lesion a patient has, our team of advanced endoscopists offers a technology known as endoscopic ultrasound (EUS). This technology makes it possible to visualize the lesion in fine detail within the esophagus by using an ultrasound device at the tip of an endoscope. It provides real-time, close-up images of the lesion.
EUS also makes it possible to take samples (biopsies) of the lesion using fine-needle aspiration. The biopsy is very safe and is accomplished with a small needle inserted through the channel of the endoscope.
Small, mucosal-based and submucosal esophageal tumors can be removed endoscopically using EMR techniques or possibly obliterated by endoscopic injection of sclerosants or by APC. Larger mass lesions, especially leiomyomas, are generally removed surgically if they are associated with severe symptoms or other complications, eg, bleeding. In many instances, the resection can now be accomplished by minimally invasive techniques.
REFERENCES