Health Centers > Cancer Health Center > Cancer of the Vulva
Cancer of the Vulva
Vulvar cancer accounts for about 4% of cancers in the female reproductive organs and 0.6% of all cancers in women. The American Cancer Society estimates that in 2005, about 3,870 cancers of the vulva will be diagnosed in the United States and about 870 women will die of this cancer. Cancer of the vulva accounts for 4.7% of malignant neoplasms in the genital tract. It is the fourth most frequent gynecologic cancer.
Cancer of the Vulva
Essentials of diagnosis
General Considerations
Pathology
¬ SQUAMOUS CELL CARCINOMA
¬ CARCINOMA OF BARTHOLIN'S GLAND
¬ BASAL CELL CARCINOMA
¬ MALIGNANT MELANOMA
¬ UNUSUAL VULVAR MALIGNANCIES
Clinical Findings
Symptoms and signs
Differential Diagnosis
Treatment
Operative Morbidity & Mortality
Follow-Up
Prognosis
Essentials of diagnosis
- Typically occurs in postmenopausal women.
- Long history of vulvar irritation with pruritus, local discomfort, and bloody discharge.
- Appearance of early lesions like that of chronic vulvar dermatitis.
- Appearance of late lesions like that of a large cauliflower, or a hard ulcerated area in the vulva.
- Biopsy necessary for diagnosis.
General Considerations
Cancer of the vulva may arise from the skin, subcutaneous tissues, glandular elements of the vulva, or the epithelium of the lower third of the vagina. Approximately 90% of these tumors are squamous cell carcinomas. Less common tumors are extramammary Paget's disease with underlying adenocarcinoma, carcinoma of Bartholin's gland, basal cell carcinoma, melanoma, sarcoma, and metastatic cancers from other sites.
Cancer of the vulva is uncommon, accounting for approximately 5% of gynecologic cancers. Vulvar cancer is more common in the poor and elderly in most parts of the world, and no race or culture is spared. Vulvar cancer is primarily a disease of postmenopausal women, with a peak incidence in women ages 60-70 years. The average age at the time of diagnosis is 65 years, and 75% of patients are older than the age of 50 years.
In general, the mean age of patients with carcinoma in situ is approximately 10 years less than that for patients with invasive cancer. Intraepithelial cancer of the vulva in women ages 20-40 years has increased remarkably in recent years, coincidentally with an increase in the incidence of diagnosis of dysplasia and carcinoma in situ of the cervix. HPV is strongly associated in younger women, though not in older women with vulvar cancer. Also, older women are more likely to have squamous hyperplasia in the tissue adjacent to the tumor.
Vulvar Cancer
Vulvar cancer is an uncommon malignancy, responsible for only 5% of all gynecologic neoplasms
Considering that cancer of the vulva is a disease of a body surface readily accessible to diagnostic procedures, early diagnosis should be the rule. This is not the case, however, and a 6- to 12-month delay in reporting symptoms of discovery of a tumor is common. Despite the advanced age of many of these patients and the frequent finding of a moderately large tumor, the disease is usually amenable to surgical therapy. In stages I and II disease, the corrected 5-year survival rate is greater than 90%. A 75% corrected 5-year survival rate for all stages of vulvar cancer is reported by most institutions.
Associated disorders found most frequently with carcinoma of the vulva are obesity, hypertension, and chronic vulvar irritation secondary to diabetes mellitus, granulomatous venereal disease, or vulvar dystrophy.
Gynecologic Cancers
Introduction
Endometrial Cancer
Ovarian Cancer
Cervical Cancer
Vulvar Cancer
Additional Issues for the Geriatric Patient
Pathology
The gross appearance of vulvar cancer depends on the origin and histologic type. These tumors spread by local extension and, with few exceptions, by lymphatic embolization. The primary route of lymphatic spread is by way of the superficial inguinal, deep femoral, and external iliac lymph nodes (Fig 49-5). Contralateral spread may occur as a result of the rich intercommunicating lymphatic system of the vulvar skin. Direct extension to the deep pelvic lymph nodes, primarily the obturator nodes, occurs in approximately 3% of patients and seems to be related to midline involvement around the clitoris, urethra, or rectum, or to cancer of a vestibular (Bartholin's) gland. Extension of the tumor to the lower and middle thirds of the vagina may also allow access of tumor cells to lymph channels leading to the deep pelvic lymph nodes.
The following sections describe the gross and histologic appearance of the various types of vulvar cancers.
A. SQUAMOUS CELL CARCINOMA
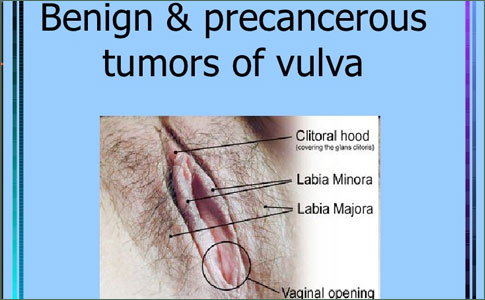
Squamous cell carcinoma is by far the most common type of tumor and most frequently involves the anterior half of the vulva. In approximately 65% of patients, the tumor arises in the labia majora and minora, and in 25% the clitoris or perineum is involved. More than one-third of tumors involve the vulva bilaterally or are midline tumors. These tumors are most frequently associated with nodal spread, particularly bilateral nodal metastases. Midline tumors that involve the perineum do not worsen the outlook unless they extend into the vagina or to the anus and rectum.
Squamous cell carcinoma of the vulva varies in appearance from a large, exophytic, cauliflowerlike lesion to a small ulcer crater superimposed on a dystrophic lesion of the vulvar skin (Figs 49-6 and 49-7). Ulcerative lesions may begin as a raised, flat, white area of hypertrophic skin that subsequently undergoes ulceration. Exophytic lesions may become extremely large, undergo necrosis, and become secondarily infected and malodorous. A third variety arises as a slightly elevated, red, velvety tumor that gradually spreads over the vulvar skin. There does not appear to be a positive correlation between the gross appearance of the tumor and either histologic grade or frequency of nodal metastases. The primary determinant of nodal metastases is tumor size.
Squamous cell cancers may be graded histologically from I to III. Grade I tumors are well differentiated, often forming keratin pearls; grade II tumors are moderately well differentiated; grade III tumors are composed of poorly differentiated cells. The extent of underlying inflammatory cell infiltration into the stroma surrounding the invasive tumor is variable. The histologic grade of the tumor may be of some significance in tumors less than 2 cm in diameter. However, the lymph node status is the most significant prognostic factor.
A variant of squamous cell carcinoma, verrucous carcinoma, is a locally invasive tumor that seldom metastasizes to regional lymph nodes. Grossly, the tumor looks like a mature condylomatous growth. It is distinguished from squamous cell cancer by histopathology of the tumor base, which reveals papillary fronds without a central core. Local recurrence is common if a wide vulvectomy is not performed; lymphadenectomy is usually not recommended.
GYNECOLOGIC NEOPLASMS
ENDOMETRIAL CANCER
¬Etiology and Pathology
¬Symptoms, Signs, and Diagnosis
¬Staging, Prognosis, and Treatment
OVARIAN CANCER
¬Etiology and Pathology
¬Symptoms, Signs, and Diagnosis
¬Treatment
CERVICAL CANCER
¬Pathology
¬Symptoms and Signs
¬Diagnosis
¬Prognosis and Treatment
VULVAR CANCER
¬Pathology
¬Symptoms, Signs, and Diagnosis
¬Prognosis
¬Treatment
VAGINAL CANCER
¬Symptoms and Signs
¬Prognosis and Treatment
FALLOPIAN TUBE CANCER
¬Symptoms, Signs, and Diagnosis
GESTATIONAL TROPHOBLASTIC DISEASE
¬Symptoms, Signs, and Diagnosis
¬Treatment
¬Etiology and Pathology
¬Symptoms, Signs, and Diagnosis
¬Staging, Prognosis, and Treatment
OVARIAN CANCER
¬Etiology and Pathology
¬Symptoms, Signs, and Diagnosis
¬Treatment
CERVICAL CANCER
¬Pathology
¬Symptoms and Signs
¬Diagnosis
¬Prognosis and Treatment
VULVAR CANCER
¬Pathology
¬Symptoms, Signs, and Diagnosis
¬Prognosis
¬Treatment
VAGINAL CANCER
¬Symptoms and Signs
¬Prognosis and Treatment
FALLOPIAN TUBE CANCER
¬Symptoms, Signs, and Diagnosis
GESTATIONAL TROPHOBLASTIC DISEASE
¬Symptoms, Signs, and Diagnosis
¬Treatment
¬Symptoms, Signs, and Diagnosis
¬Staging, Prognosis, and Treatment
OVARIAN CANCER
¬Etiology and Pathology
¬Symptoms, Signs, and Diagnosis
¬Treatment
CERVICAL CANCER
¬Pathology
¬Symptoms and Signs
¬Diagnosis
¬Prognosis and Treatment
VULVAR CANCER
¬Pathology
¬Symptoms, Signs, and Diagnosis
¬Prognosis
¬Treatment
VAGINAL CANCER
¬Symptoms and Signs
¬Prognosis and Treatment
FALLOPIAN TUBE CANCER
¬Symptoms, Signs, and Diagnosis
GESTATIONAL TROPHOBLASTIC DISEASE
¬Symptoms, Signs, and Diagnosis
¬Treatment
¬Staging, Prognosis, and Treatment
OVARIAN CANCER
¬Etiology and Pathology
¬Symptoms, Signs, and Diagnosis
¬Treatment
CERVICAL CANCER
¬Pathology
¬Symptoms and Signs
¬Diagnosis
¬Prognosis and Treatment
VULVAR CANCER
¬Pathology
¬Symptoms, Signs, and Diagnosis
¬Prognosis
¬Treatment
VAGINAL CANCER
¬Symptoms and Signs
¬Prognosis and Treatment
FALLOPIAN TUBE CANCER
¬Symptoms, Signs, and Diagnosis
GESTATIONAL TROPHOBLASTIC DISEASE
¬Symptoms, Signs, and Diagnosis
¬Treatment
OVARIAN CANCER
¬Etiology and Pathology
¬Symptoms, Signs, and Diagnosis
¬Treatment
CERVICAL CANCER
¬Pathology
¬Symptoms and Signs
¬Diagnosis
¬Prognosis and Treatment
VULVAR CANCER
¬Pathology
¬Symptoms, Signs, and Diagnosis
¬Prognosis
¬Treatment
VAGINAL CANCER
¬Symptoms and Signs
¬Prognosis and Treatment
FALLOPIAN TUBE CANCER
¬Symptoms, Signs, and Diagnosis
GESTATIONAL TROPHOBLASTIC DISEASE
¬Symptoms, Signs, and Diagnosis
¬Treatment
¬Etiology and Pathology
¬Symptoms, Signs, and Diagnosis
¬Treatment
CERVICAL CANCER
¬Pathology
¬Symptoms and Signs
¬Diagnosis
¬Prognosis and Treatment
VULVAR CANCER
¬Pathology
¬Symptoms, Signs, and Diagnosis
¬Prognosis
¬Treatment
VAGINAL CANCER
¬Symptoms and Signs
¬Prognosis and Treatment
FALLOPIAN TUBE CANCER
¬Symptoms, Signs, and Diagnosis
GESTATIONAL TROPHOBLASTIC DISEASE
¬Symptoms, Signs, and Diagnosis
¬Treatment
¬Symptoms, Signs, and Diagnosis
¬Treatment
CERVICAL CANCER
¬Pathology
¬Symptoms and Signs
¬Diagnosis
¬Prognosis and Treatment
VULVAR CANCER
¬Pathology
¬Symptoms, Signs, and Diagnosis
¬Prognosis
¬Treatment
VAGINAL CANCER
¬Symptoms and Signs
¬Prognosis and Treatment
FALLOPIAN TUBE CANCER
¬Symptoms, Signs, and Diagnosis
GESTATIONAL TROPHOBLASTIC DISEASE
¬Symptoms, Signs, and Diagnosis
¬Treatment
¬Treatment
CERVICAL CANCER
¬Pathology
¬Symptoms and Signs
¬Diagnosis
¬Prognosis and Treatment
VULVAR CANCER
¬Pathology
¬Symptoms, Signs, and Diagnosis
¬Prognosis
¬Treatment
VAGINAL CANCER
¬Symptoms and Signs
¬Prognosis and Treatment
FALLOPIAN TUBE CANCER
¬Symptoms, Signs, and Diagnosis
GESTATIONAL TROPHOBLASTIC DISEASE
¬Symptoms, Signs, and Diagnosis
¬Treatment
CERVICAL CANCER
¬Pathology
¬Symptoms and Signs
¬Diagnosis
¬Prognosis and Treatment
VULVAR CANCER
¬Pathology
¬Symptoms, Signs, and Diagnosis
¬Prognosis
¬Treatment
VAGINAL CANCER
¬Symptoms and Signs
¬Prognosis and Treatment
FALLOPIAN TUBE CANCER
¬Symptoms, Signs, and Diagnosis
GESTATIONAL TROPHOBLASTIC DISEASE
¬Symptoms, Signs, and Diagnosis
¬Treatment
¬Pathology
¬Symptoms and Signs
¬Diagnosis
¬Prognosis and Treatment
VULVAR CANCER
¬Pathology
¬Symptoms, Signs, and Diagnosis
¬Prognosis
¬Treatment
VAGINAL CANCER
¬Symptoms and Signs
¬Prognosis and Treatment
FALLOPIAN TUBE CANCER
¬Symptoms, Signs, and Diagnosis
GESTATIONAL TROPHOBLASTIC DISEASE
¬Symptoms, Signs, and Diagnosis
¬Treatment
¬Symptoms and Signs
¬Diagnosis
¬Prognosis and Treatment
VULVAR CANCER
¬Pathology
¬Symptoms, Signs, and Diagnosis
¬Prognosis
¬Treatment
VAGINAL CANCER
¬Symptoms and Signs
¬Prognosis and Treatment
FALLOPIAN TUBE CANCER
¬Symptoms, Signs, and Diagnosis
GESTATIONAL TROPHOBLASTIC DISEASE
¬Symptoms, Signs, and Diagnosis
¬Treatment
¬Diagnosis
¬Prognosis and Treatment
VULVAR CANCER
¬Pathology
¬Symptoms, Signs, and Diagnosis
¬Prognosis
¬Treatment
VAGINAL CANCER
¬Symptoms and Signs
¬Prognosis and Treatment
FALLOPIAN TUBE CANCER
¬Symptoms, Signs, and Diagnosis
GESTATIONAL TROPHOBLASTIC DISEASE
¬Symptoms, Signs, and Diagnosis
¬Treatment
¬Prognosis and Treatment
VULVAR CANCER
¬Pathology
¬Symptoms, Signs, and Diagnosis
¬Prognosis
¬Treatment
VAGINAL CANCER
¬Symptoms and Signs
¬Prognosis and Treatment
FALLOPIAN TUBE CANCER
¬Symptoms, Signs, and Diagnosis
GESTATIONAL TROPHOBLASTIC DISEASE
¬Symptoms, Signs, and Diagnosis
¬Treatment
VULVAR CANCER
¬Pathology
¬Symptoms, Signs, and Diagnosis
¬Prognosis
¬Treatment
VAGINAL CANCER
¬Symptoms and Signs
¬Prognosis and Treatment
FALLOPIAN TUBE CANCER
¬Symptoms, Signs, and Diagnosis
GESTATIONAL TROPHOBLASTIC DISEASE
¬Symptoms, Signs, and Diagnosis
¬Treatment
¬Pathology
¬Symptoms, Signs, and Diagnosis
¬Prognosis
¬Treatment
VAGINAL CANCER
¬Symptoms and Signs
¬Prognosis and Treatment
FALLOPIAN TUBE CANCER
¬Symptoms, Signs, and Diagnosis
GESTATIONAL TROPHOBLASTIC DISEASE
¬Symptoms, Signs, and Diagnosis
¬Treatment
¬Symptoms, Signs, and Diagnosis
¬Prognosis
¬Treatment
VAGINAL CANCER
¬Symptoms and Signs
¬Prognosis and Treatment
FALLOPIAN TUBE CANCER
¬Symptoms, Signs, and Diagnosis
GESTATIONAL TROPHOBLASTIC DISEASE
¬Symptoms, Signs, and Diagnosis
¬Treatment
¬Prognosis
¬Treatment
VAGINAL CANCER
¬Symptoms and Signs
¬Prognosis and Treatment
FALLOPIAN TUBE CANCER
¬Symptoms, Signs, and Diagnosis
GESTATIONAL TROPHOBLASTIC DISEASE
¬Symptoms, Signs, and Diagnosis
¬Treatment
¬Treatment
VAGINAL CANCER
¬Symptoms and Signs
¬Prognosis and Treatment
FALLOPIAN TUBE CANCER
¬Symptoms, Signs, and Diagnosis
GESTATIONAL TROPHOBLASTIC DISEASE
¬Symptoms, Signs, and Diagnosis
¬Treatment
VAGINAL CANCER
¬Symptoms and Signs
¬Prognosis and Treatment
FALLOPIAN TUBE CANCER
¬Symptoms, Signs, and Diagnosis
GESTATIONAL TROPHOBLASTIC DISEASE
¬Symptoms, Signs, and Diagnosis
¬Treatment
¬Symptoms and Signs
¬Prognosis and Treatment
FALLOPIAN TUBE CANCER
¬Symptoms, Signs, and Diagnosis
GESTATIONAL TROPHOBLASTIC DISEASE
¬Symptoms, Signs, and Diagnosis
¬Treatment
¬Prognosis and Treatment
FALLOPIAN TUBE CANCER
¬Symptoms, Signs, and Diagnosis
GESTATIONAL TROPHOBLASTIC DISEASE
¬Symptoms, Signs, and Diagnosis
¬Treatment
FALLOPIAN TUBE CANCER
¬Symptoms, Signs, and Diagnosis
GESTATIONAL TROPHOBLASTIC DISEASE
¬Symptoms, Signs, and Diagnosis
¬Treatment
¬Symptoms, Signs, and Diagnosis
GESTATIONAL TROPHOBLASTIC DISEASE
¬Symptoms, Signs, and Diagnosis
¬Treatment
GESTATIONAL TROPHOBLASTIC DISEASE
¬Symptoms, Signs, and Diagnosis
¬Treatment
¬Symptoms, Signs, and Diagnosis
¬Treatment
¬Treatment
An attempt has been made to define a group of early vulvar cancers that might be described as microinvasive cancer and that exhibit little tendency for local recurrence or nodal metastases. Depth of stromal penetration has proved to be the key factor in determining invasive potential of the tumor. Early authors accepted 5 mm or less of dermal invasion as the definition of microinvasion, but this has not been universally accepted. A task force of the International Society for the Study of Vulvar Diseases suggested that the term "microinvasive cancer of the vulva" be discarded. The ISSVD defined stage IA carcinoma of the vulva as a single lesion measuring 2 cm or less in diameter and exhibiting one focus of invasion to a depth of 1 mm or less. The depth of invasion was measured from the epidermal-stromal junction of the most superficial dermal papilla to the deepest point of tumor invasion.
B. CARCINOMA OF BARTHOLIN'S GLAND
Carcinoma of Bartholin's gland accounts for approximately 1% of vulvar cancers, and although rare, is the most common site for vulvar adenocarcinoma. Approximately 50% of Bartholin's gland tumors are squamous cell carcinomas. Other types of tumors arising in the Bartholin's glands are adenocarcinoma, adenoid cystic (an adenocarcinoma with specific histologic and clinical characteristics), adenosquamous, and transitional cell.
Because it may be difficult to differentiate by clinical examination a tumor of Bartholin's gland or duct from a benign Bartholin's cyst, any woman older than age 40 years should undergo biopsy to rule out cancer, as inflammatory disease is not common in this age group. Because of its location deep in the substance of the labium, a tumor may impinge on the rectum and directly spread into the ischiorectal fossa. Consequently, these tumors have access to lymphatic channels draining directly to the deep pelvic lymph nodes as well as to the superficial channels draining to the inguinal lymph nodes.
C. BASAL CELL CARCINOMA
Basal cell carcinomas account for 1-2% of vulvar cancers. Most tumors are small elevated lesions with an ulcerated center and rolled edges. Some are described as pigmented tumors, moles, or simply pruritic maculopapular eruptions. These tumors arise almost exclusively in the skin of the labia majora, although occasionally a tumor can be found elsewhere in the vulva. The tumor is derived from primordial basal cells in the epidermis or hair follicles and is characterized by slow growth, local infiltration, and a tendency to recur if not totally excised. Most basal cell carcinomas of the vulva are of the primordial histologic type. Other histologic varieties that may be found are the pilar, morphealike, superficially spreading, adenoid, and pigmented cell tumors.
On microscopic examination the typical tumor consists of nodular masses and lobules of closely packed, uniform-appearing basaloid cells with scant cytoplasm and spherical or oval dark nuclei. Peripheral margination by columnar cells is usually prominent. In larger tumor nodules, there may be areas of central degeneration and necrosis.
If a sufficiently wide local excision is not performed, there is a tendency for local recurrence, estimated to be approximately 20%. If a basal-squamous cell-type tumor is diagnosed, appropriate therapy for invasive epidermoid cancer of the vulva should be undertaken.
D. MALIGNANT MELANOMA
Approximately 5% of vulvar cancers are malignant melanomas, the second most common vulvar cancer. Because only 0.1% of all nevi in women are on vulvar skin, the disproportionate frequency of occurrence of melanoma in this area may be a result of the fact that nearly all vulvar nevi are of the junctional variety. Malignant melanoma most commonly arises in the region of the labia minora and clitoris, and there is a tendency for superficial spread toward the urethra and vagina. A nonpigmented melanoma may closely resemble squamous cell carcinoma on clinical examination. A darkly pigmented, raised lesion at the mucocutaneous junction is a characteristic finding; however, the degree of melanin pigmentation is variable, and amelanotic lesions do occur. The lesion spreads primarily through lymphatic channels and tends to metastasize early in the course of the disease; local or remote cutaneous satellite lesions may be found. In contrast to squamous cell cancers, melanoma is staged according to depth of invasion. All small pigmented lesions of the vulva are suspect and should be removed by excision biopsy with a 0.5- to 1-cm margin of normal skin. In the case of large tumors, the diagnosis should be confirmed by a generous biopsy.
E. UNUSUAL VULVAR MALIGNANCIES
Sarcomas of the vulva constitute a variety of malignant neoplasms that account for 1-2% of vulvar cancers. The most common is leiomyosarcoma, followed in frequency of occurrence by the fibrous histiocytoma group and an array of other sarcomas. Clinically, sarcoma may present as a subcutaneous nodule or may be exophytic and fleshy. Prognosis is usually poor and depends on histologic type, extent of local invasion, and treatment. In general, radical vulvectomy and regional lymphadenectomy are indicated, with the exception of tumors such as dermatofibrosarcoma protuberans, which is a locally aggressive tumor that tends to recur locally but does not metastasize.
Adenocarcinoma of the vulva is exceptionally rare unless it arises from the Bartholin's gland or the urethra. Primary cancer of the breast from ectopic breast tissue has been reported. Rarely, a malignant tumor will arise from a vulvar sweat gland.
Metastatic cancers of the vulva constitute 8% of all vulvar tumors. They usually originate from a genital tract tumor, and 18% arise from the kidney or urethra. Advanced cervical cancer is the most common primary tumor. Other primary tumors have been reported, including malignant melanoma, choriocarcinoma, and adenocarcinoma of the rectum or breast. Cloacogenic carcinoma is primarily an anorectal neoplasm, occurring twice as often in women than in men; it may arise in anal ducts and present as a submucosal mass.
Metastatic epidermoid cancer tends to form nests of cells within the dermis. Adenocarcinoma, regardless of the primary site, invades the surface squamous epithelium. Because these tumors are a manifestation of advanced disease, the prognosis is uniformly grave.