Anorectal fistulas
Anorectal fistulas are generally uncommon, with some studies reporting an incidence of 8.6 per 100,000 (16). The leading causes are nonspecific in 90% of patients. Fistulas may be associated with Crohn’s disease (Figure 2), anal fissures, postoperative and perirectal/anal trauma, and infections such as a sequelae of anorectal abscesses of nonspecific anal origin (17).
There is a slight male predilection, and the average age at diagnosis is 38 years.
Anorectal fistulas can develop in other medical disorders such as anorectal malignancy, lymphogranuloma venereum, radiation proctitis, actinomycosis, tuberculosis, and leukemia.
The classification of fistulas is divided into 4 common types (Table II); however, they can have a complex anatomy, with 1 or more extensions and accessory tracts possible.
Patients with symptomatic anorectal fistulas usually require surgical management. Anal fistulas complicating Crohn’s disease should be initially managed with medical therapy, which may include total parenteral nutrition, metronidazole, or a recently available option, IV infliximab, a tumor necrosis factor-α inhibitor. If in this patient population there is no healing with medical therapy, then surgical treatment should be considered.
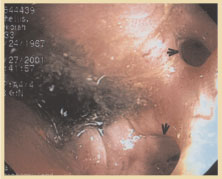 Figure 2. Endoscopic appearance of 2 rectovaginal fistulas in a patient with Crohn’s disease. The goal of surgical management of anorectal fistulas is to eradicate the fistula while preserving fecal continence. Surgery usually entails an examination under anesthesia whereby the fistula is gently probed to define the anatomy. Intersphincteric fistulas are managed by a primary fistulotomy; the base of the wound is then curetted and left open to heal by secondary intention facilitated by fiber therapy and sitz baths.
Figure 2. Endoscopic appearance of 2 rectovaginal fistulas in a patient with Crohn’s disease. The goal of surgical management of anorectal fistulas is to eradicate the fistula while preserving fecal continence. Surgery usually entails an examination under anesthesia whereby the fistula is gently probed to define the anatomy. Intersphincteric fistulas are managed by a primary fistulotomy; the base of the wound is then curetted and left open to heal by secondary intention facilitated by fiber therapy and sitz baths.
Transsphincteric fistulas are usually divided into low and high fistulas. Low fistulas are managed by a primary fistulotomy with maintenance of good preoperative sphincter function. High transsphincteric and anterior fistulas are managed with a conservative approach whereby a cutting section is often performed.
This procedure involves placing a reactive suture or elastic through the fistulous tract and tightening it sequentially until it cuts through the tract. A relatively new therapy involves the injection of fibrin glue, which may eradicate fistulas in as many as 60% of patients with complicated tracts (18).
Deepak V. Gopal, MD, FRCP (C)
Assistant Professor of Medicine
Division of Gastroenterology
Oregon Health & Science University
Portland VA Medical Center
Portland, Oregon
REFERENCES
1. Schrock TR. Examination and diseases of the anorectum. In: Feldman M, Scharschmidt BF, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease.
2. Barnett JL. Anorectal diseases. In: Yamada T, Alpers DH, Laine L, et al, eds. Textbook of Gastroenterology. Vol 2. 3rd ed. Philadelphia, Pa: Lippincott Williams & Wilkins; 1999:2083 - 2107.
3. Johanson JF, Sonnenberg A. The prevalence of hemorrhoids and chronic constipation: an epidemiological study. Gastroenterology. 1990;98:380 - 386.
4. Breen E, Bleday R. Clinical features of hemorrhoids. [UpToDate Clinical Reference on CD-ROM & Online Web site.] December 2001.
5. Haas PA, Fox TA, Haas G. The pathogenesis of hemorrhoids. Dis Colon Rectum. 1984;27:442 - 450.
6. Bleday R, Breen E. Treatment of hemorrhoids. [UpToDate Clinical Reference on CD-ROM & Online Web site.] December 2001.
7. MacRae HM, McLeod RS. Comparison of hemorrhoidal treatments: a meta-analysis. Can J Surg. 1997;40:14 - 17.
8. Reis Neto JA, Quilici FA, Cordeiro F, Reis JA. Open versus semi-open hemorrhoidectomy: a random trial. Int Surg. 1992;77:84 - 90.
9. Khubchandani M. Results of Whitehead operation. Dis Colon Rectum. 1984;27:730 - 732.
10. Breen E, Bleday R. Anal fissures. [UpToDate Clinical Reference on CD-ROM & Online Web site.] December 2001.
11. Lund JN, Scholefield JH. Aetiology and treatment of anal fissure. Br J Surg. 1996;83:1335 - 1344.
12. Shub HA, Salvati EP, Rubin RJ. Conservative treatment of anal fissure: an unselected, retrospective, and continuous study. Dis Colon Rectum. 1978;21: 582 - 583.
13. Brisinda G, Maria G, Bentivoglio AR, et al. A comparison of injections of botulinum toxin and topical nitroglycerin ointment for the treatment of chronic anal fissure. N Engl J Med. 1999; 341:65 - 69.
14. Cook TA, Humphreys MM, McC Mortensen NJ. Oral nifedipine reduces resting anal pressure and heals chronic anal fissure. Br J Surg. 1999;86: 1269 - 1273.
15. Lewis TH, Corman ML, Prager ED, Robertson WG. Long-term results of open and closed sphincterotomy for anal fissure. Dis Colon Rectum. 1988;31: 368 - 371.
16. Breen E, Bleday R. Anal abscesses and fistulas. [UpToDate Clinical Reference on CD-ROM & Online Web site.] December 2001.
17. Nordgren S, Fasth S, Hulten L. Anal fistulas in Crohn's disease: incidence and outcome of surgical treatment. Int J Colorectal Dis. 1992;7:214 - 218.
18. Venkatesh KS, Ramanujam P. Fibrin glue application in the treatment of recurrent anorectal fistulas. Dis Colon Rectum. 1999;42:1136 - 1139.
19. Gopal DV, Young C, Katon RM. Solitary rectal ulcer syndrome presenting with rectal prolapse, severe mucorrhea, and eroded polypoid hyperplasia: case report and review of the literature. Can J Gastroenterol. 2001;15:479 - 483.
20. Mackle EJ, Parks TG. The pathogenesis and patho-physiology of rectal prolapse and solitary rectal ulcer syndrome. Clin Gastroenterol. 1986;15: 985 - 1001.
21. Gopal DV, Faigel DO. Rectal endoscopic ultrasound - a review of clinical applications. Endoscopic ultrasonography and therapeutic indications. Series #2. Pract Gastroenterol. 2000;24:24 - 34.
22. Robson K, Lembo AJ. Fecal incontinence. Chopra S, La Mont T, eds. [UpToDate Clinical Reference on CD-ROM & Online Web site.] December 2001.
23. Nostrant TT. Radiation injury. In: Yamada T, Alpers DH, Laine L, et al, eds. Textbook of Gastroenterology. Vol 2. 3rd ed. Philadelphia, Pa: Lippincott Williams & Wilkins; 1999:2611 - 2612.
24. Swaroop VS, Gostout CJ. Endoscopic treatment of chronic radiation proctopathy. J Clin Gastroenterol. 1998;27:36 - 40.
25. Bonis P, Breen E, Bleday R. Approach to the patient with anal pruritus. [UpToDate Clinical Reference on CD-ROM & Online Web site.] December 2001.
26. American Joint Committee on Cancer. Manual for Staging of Cancer. 4th ed. Philadelphia, Pa: JB Lippincott; 1992:75 - 79.
27. Magdeburg B, Fried M, Meyenberger C. Endoscopic ultrasonography in the diagnosis, staging, and follow-up of anal carcinomas. Endoscopy. 1999;31:359 - 364.