What is Fibromyalgia
The hallmark of fibromyalgia (FM) includes the presence of multiple tender points at specific locations over the body, combined with the report of widespread musculoskeletal pain. A good analogy is to consider pain as a radio signal.
If the volume control on the receiver is broken and broadcasts only at a greatly amplified sound level, an otherwise normal listening experience will become difficult to tolerate. It is the same type of experience with pain in FM; even typically nonpainful stimuli like a gentle hug can cause discomfort because of pain amplification.
This phenomenon is caused in large part by central sensitization, and in fact, many researchers believe the central nervous system is the key factor in the pathology of FM.
Like most chronic illnesses, the symptoms of FM extend far beyond the defining criteria. In addition to pain, many patients also report the following co-morbidities (overlapping but separate disorders or symptoms):
- Fatigue
- Muscle and joint stiffness
- Insomnia
- Restless Legs Syndrome (RLS)
- Balance issues, including orthostatic hypotension and dysautonomia
- Headaches, including migraine headaches• Cognitive lapses
- Raynaud’s Phenomenon
- Autoimmune disorders such as Sjögren’s Syndrome and rheumatoid arthritis
- Visual, auditory, tactile, and olfactory hypersensitivities
- Irritable bowel and irritable bladder
- Pelvic pain, endometriosis, vulvodynia
- Depression and anxiety disorders
- Temporomandibular joint dysfunction
The symptoms of FM may improve, may worsen, or may be continual, but the disorder is extremely unlikely to completely go away. Periods when symptoms worsen are termed flares and are often brought on by physical overexertion or stress. Many people with FM find that, at least some of the time, their illness prevents them from engaging in common everyday activities, such as traveling in a car for prolonged periods and climbing stairs.
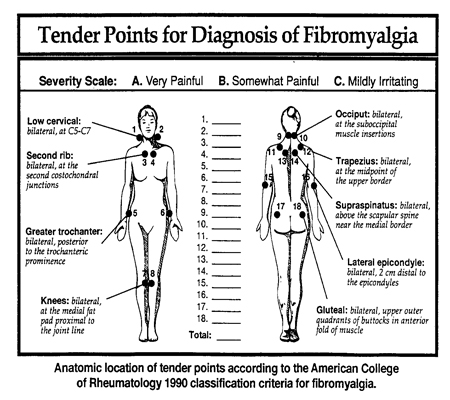
Classification criteria for fibromyalgia as published by the American College of Rheumatology:
- History of widespread pain for at least three months
- Pain on both sides of the body, and above and below the waist
- Axial skeletal pain must be present (cervical spine, anterior chest, thoracic spine, or low back)
- Pain in 11 of 18 tender point sites on digital palpation with an approximate pressure of 4 kg/cm
- Patient must state that the palpation is ‘painful’; ‘tender’ does not qualify
 In addition to the above American College of Rheumatology classification criteria, most patients (greater than 75%) also describe:
In addition to the above American College of Rheumatology classification criteria, most patients (greater than 75%) also describe:
- Awakening from a night of sleep still feeling tired and not refreshed
- Fatigue
- Morning stiffness
Ultimate diagnosis may be one of exclusion after differentials have been ruled out.
The disorder can be debilitating and often has a serious impact on family relationships, social friendships, and the ability to stay employed. It is understandable that life satisfaction levels suffer when someone cannot participate in what is considered a normal lifestyle. As is true with most chronic pain conditions, depression and anxiety are a common response to FM symptoms. Unfortunately, some medical providers continue to treat FM as only a psychosomatic disorder despite more and more research confirming FM is, in fact, physical.
 There are some further points to remember about this disorder. First, FM is not limited to the musculoskeletal system; research has shown brain and spinal cord involvement. Second, although some persons with FM may first experience primary immune system disorders such as rheumatoid arthritis, systemic lupus erythematosus (SLE), or Sjögren’s Syndrome, FM is not in itself an autoimmune disease. Third, we know this disorder is not the same as Chronic Fatigue Immune Dysfunction Syndrome (CFIDS) since people with FM have chemical hallmarks in their spinal column fluid that are not present in CFIDS. Fourth, FM is not a mental illness. Studies have shown there is no higher incidence of mental illness in FM than in many other chronic pain populations.
There are some further points to remember about this disorder. First, FM is not limited to the musculoskeletal system; research has shown brain and spinal cord involvement. Second, although some persons with FM may first experience primary immune system disorders such as rheumatoid arthritis, systemic lupus erythematosus (SLE), or Sjögren’s Syndrome, FM is not in itself an autoimmune disease. Third, we know this disorder is not the same as Chronic Fatigue Immune Dysfunction Syndrome (CFIDS) since people with FM have chemical hallmarks in their spinal column fluid that are not present in CFIDS. Fourth, FM is not a mental illness. Studies have shown there is no higher incidence of mental illness in FM than in many other chronic pain populations.
The epidemiology of fibromyalgia is poorly defined. The incidence of fibromyalgia has not been determined using a large population base. Previous studies based on prevalence data demonstrated that females are 7 times more likely to have fibromyalgia than males and that the peak age for females is during the childbearing years.
###
Females are more likely to be diagnosed with fibromyalgia than males, although to a substantially smaller degree than previously reported, and there are strong associations for comorbid conditions that are commonly thought to be associated with fibromyalgia.
###
J Clin Rheumatol. 2006 Jun;12(3):124-8.
The incidence of fibromyalgia and its associated comorbidities: a population-based retrospective cohort study based on International Classification of Diseases, 9th Revision codes.
Weir PT, Harlan GA, Nkoy FL, Jones SS, Hegmann KT, Gren LH, Lyon JL.
Overall, it is important to remember that FM is not a catchall diagnosis; it is a chronic, nondegenerative, noninflammatory disorder with an accepted diagnostic criteria.
GLOBAL STATISTICS AND ECONOMIC RESULTS
Approximately 15 million persons in the United States have been diagnosed with FM. It can occur at any point in life but is most commonly diagnosed in middle age. The disorder strikes men, women, and children of all races, although women are diagnosed with FM eight to nine times more often than men. That ratio may change since many returning Gulf War veterans who experienced the chronic stress of being in war and known chemical and toxin exposure are exhibiting symptoms similar to, and which in fact may be, FM.
Since the 1990 College of Rheumatology classification criteria for FM was established, epidemiological studies estimate that the disorder occurs from 1.3 percent to 7.3 percent in the population worldwide. At least fifteen different countries have recorded criteria-based cases of FM, indicating that it is not limited to industrialized countries, and further, affects people of all ages, races, and ethnicities. Despite the outward appearance of normality, persons with this disorder often have difficulty staying in the workforce, and a downward spiral toward work disability is not uncommon. This is especially the case for medically undertreated persons and those who experience many of the overlapping comorbidities of FM. Approximately 16 percent of FM-diagnosed U.S. citizens receive Social Security benefits, compared to 2.2 percent of the general U.S. population. FM also represents a liability to medical systems in the United States and worldwide. The direct cost of FM medical care in the United States alone is $20 billion annually and the average rate of medical services in the United States for each patient nears $10,000 yearly.
HISTORY
Spinal Irritation is characterized by multiple tender spots distributed over the
female body, probably caused by sexual excess. . . . leeches to the inside of the nos-
trils are remarkably efficacious. . . .
- William A. Hammond, Spinal Irritation, 1886
Many would argue that throughout history the medical ailments suffered mainly by women have been met with medical arrogance and disrespect. FM is no different, as the above quote so well demonstrates. FM is an ancient disorder, with a long history of medical speculation as to its source, contributing factors, and potential treatments. Medical descriptions of symptoms indicating FM can be found dating back to the sixteenth century.
The differences between rheumatic conditions involving joint deformity, termed articular rheumatism, and painful but nondeforming muscular rheumatism were recorded at that time. In the early to mid-1800s, a surgeon named William Balfour from Edinburgh, Scotland, and later the physician François Valleix in Paris, independently described unusually painful areas in patients with muscular rheumatism that produced shooting pain when palpated. Fibrositis was the term that preceded fibromyalgia. It first came into use in 1904 when English neurologist Sir William Gowers wrote a medical paper on low back pain. He speculated that low back tenderness was due to inflammatory changes in muscle fiber tissue and discussed for the first time the concept of pain amplification, as well as the possible contribution of disrupted sleep and fatigue to diffuse rheumatic muscle pain. However, subsequent studies of muscle biopsies failed to find traditional indications of inflammation, and the term fibrositis was then considered a misnomer. At the turn of the twentieth century, physician Sir William Osler coined the term myalgia and speculated that the pain of muscular rheumatism involved “neuralgia of the sensory nerves of the muscles.” World War II saw an increase in the diagnosis of fibrositis in British soldiers, with 70 percent of all rheumatic patients in British army hospitals diagnosed with the condition.
Over time, the terms fibrositis, fibromyositis, muscular rheumatism, and even “tender lady syndrome” have all been used to describe this disorder. In 1973 the researcher Philip Hench first introduced the term fibromyalgia, which more accurately describes the symptoms. This current term is referenced by the following medical root words: fibra (Latin for fiber), myo (Greek for muscle), and algos (Greek for pain). Researchers such as Muhammad B. Yunus, Robert M. Bennett, I. Jon Russell, and others, seeking to clearly define FM in the 1980s, proposed the need for a unified classification system. In 1990, following a rigorous multisite research study, the American College of Rheumatology published a formal “Criteria for the Classification of Fibromyalgia.” The American Medical Association recognized FM as a true illness and as a major cause of disability in 1987; the World Health Organization followed with the same recognition in 1992.
###
Fibromyalgia (fie-bro-my-AL-gee-a), also referred to as FM, is increasingly being recognized as a real illness. This is a blessing to the many patients whose symptoms were once met with disbelief from health-care professionals and a lack of understanding from family, friends, and coworkers.
Thankfully, today the majority of health-care providers agree FM is a real disorder and the discrimination is finally waning. New clinicians coming out of school have benefited from updated training based on solid research findings; they are knowledgeable about FM, understand the American College of Rheumatology’s diagnostic guidelines, and are consequently more likely to correctly diagnose this disorder. FM has specific signs and symptoms that occur together, so it is sometimes referred to as a syndrome. However, a more recent confluence of objective research findings has compelled researchers to label FM a disorder rather than a syndrome. A disorder can be defined as a set of symptoms that are clearly connected by objective, reproducible pathophysiologic changes.
A syndrome is a broader term used earlier in the understanding of an illness when the underlying abnormalities are not as well understood.
###
Kim D. Jones and
Janice H. Hoffman
Library of Congress Cataloging-in-Publication Data