Findings point toward one of first therapies for Lou Gehrig’s disease
Researchers have determined that a copper compound known for decades may form the basis for a therapy for amyotrophic lateral sclerosis (ALS), or Lou Gehrig’s disease.
In a new study just published in the Journal of Neuroscience, scientists from Australia, the United States (Oregon), and the United Kingdom showed in laboratory animal tests that oral intake of this compound significantly extended the lifespan and improved the locomotor function of transgenic mice that are genetically engineered to develop this debilitating and terminal disease.
In humans, no therapy for ALS has ever been discovered that could extend lifespan more than a few additional months. Researchers in the Linus Pauling Institute at Oregon State University say this approach has the potential to change that, and may have value against Parkinson’s disease as well.
“We believe that with further improvements, and following necessary human clinical trials for safety and efficacy, this could provide a valuable new therapy for ALS and perhaps Parkinson’s disease,” said Joseph Beckman, a distinguished professor of biochemistry and biophysics in the OSU College of Science.
“I’m very optimistic,” said Beckman, who received the 2012 Discovery Award from the OHSU Medical Research Foundation as the leading medical researcher in Oregon.
ALS was first identified as a progressive and fatal neurodegenerative disease in the late 1800s and gained international recognition in 1939 when it was diagnosed in American baseball legend Lou Gehrig. It’s known to be caused by motor neurons in the spinal cord deteriorating and dying, and has been traced to mutations in copper, zinc superoxide dismutase, or SOD1. Ordinarily, superoxide dismutase is an antioxidant whose proper function is essential to life.
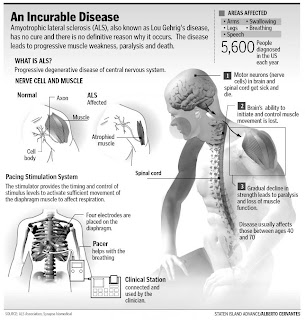
What is ALS?
Amyotrophic lateral sclerosis (ALS), often referred to as “Lou Gehrig’s Disease,” is a progressive neurodegenerative disease that affects nerve cells in the brain and the spinal cord. Motor neurons reach from the brain to the spinal cord and from the spinal cord to the muscles throughout the body. The progressive degeneration of the motor neurons in ALS eventually leads to their death. When the motor neurons die, the ability of the brain to initiate and control muscle movement is lost. With voluntary muscle action progressively affected, patients in the later stages of the disease may become totally paralyzed.
A-myo-trophic comes from the Greek language. “A” means no or negative. “Myo” refers to muscle, and “Trophic” means nourishment - “No muscle nourishment.” When a muscle has no nourishment, it “atrophies” or wastes away. “Lateral” identifies the areas in a person’s spinal cord where portions of the nerve cells that signal and control the muscles are located. As this area degenerates it leads to scarring or hardening (“sclerosis”) in the region.
As motor neurons degenerate, they can no longer send impulses to the muscle fibers that normally result in muscle movement. Early symptoms of ALS often include increasing muscle weakness, especially involving the arms and legs, speech, swallowing or breathing. When muscles no longer receive the messages from the motor neurons that they require to function, the muscles begin to atrophy (become smaller). Limbs begin to look “thinner” as muscle tissue atrophies.
 When SOD1 is lacking its metal co-factors, it “unfolds” and becomes toxic, leading to the death of motor neurons. The metals copper and zinc are important in stabilizing this protein, and can help it remain folded more than 200 years.
When SOD1 is lacking its metal co-factors, it “unfolds” and becomes toxic, leading to the death of motor neurons. The metals copper and zinc are important in stabilizing this protein, and can help it remain folded more than 200 years.
“The damage from ALS is happening primarily in the spinal cord and that’s also one of the most difficult places in the body to absorb copper,” Beckman said. “Copper itself is necessary but can be toxic, so its levels are tightly controlled in the body. The therapy we’re working toward delivers copper selectively into the cells in the spinal cord that actually need it. Otherwise, the compound keeps copper inert.”
“This is a safe way to deliver a micronutrient like copper exactly where it is needed,” Beckman said.
By restoring a proper balance of copper into the brain and spinal cord, scientists believe they are stabilizing the superoxide dismutase in its mature form, while improving the function of mitochondria. This has already extended the lifespan of affected mice by 26 percent, and with continued research the scientists hope to achieve even more extension.
The compound that does this is called copper (ATSM), has been studied for use in some cancer treatments, and is relatively inexpensive to produce.
“In this case, the result was just the opposite of what one might have expected,” said Blaine Roberts, lead author on the study and a research fellow at the University of Melbourne, who received his doctorate at OSU working with Beckman.
“The treatment increased the amount of mutant SOD, and by accepted dogma this means the animals should get worse,” he said. “But in this case, they got a lot better. This is because we’re making a targeted delivery of copper just to the cells that need it.
Lou Gehrig’s disease damages motor neurons in the brain and spinal cord. Motor neurons are nerve cells that control muscle movement. Upper motor neurons send messages from the brain to the spinal cord, and lower motor neurons send messages from the spinal cord to the muscles. Motor neurons are an important part of the body’s neuromuscular system.
The neuromuscular system enables our bodies to move and is made up of the brain, many nerves, and muscles. Things that we do every day - like breathing, walking, running, lifting stuff, and even reaching for a glass of water - are all controlled by the neuromuscular system.
Here’s how the neuromuscular system works: If you want to make a fist, your brain first sends signals through upper motor neurons to the area in your spinal cord that controls your hand muscles. Then lower motor neurons in your spinal cord signal the muscles in your hand to move and make a fist.
Over time, Lou Gehrig’s disease causes these motor neurons in the brain and spinal cord to shrink and disappear, so that the muscles no longer receive signals to move. As a result, the muscles become smaller and weaker. Gradually the body becomes paralyzed, which means that the muscles no longer work.
However, someone with ALS, even at an advanced stage, can still see, hear, smell, and feel touch. The nerves that carry feelings of hot, cold, pain, pressure, or even being tickled, are not affected by Lou Gehrig’s disease. In some people with ALS, the parts of the brain that allow us to think, remember, and learn also are affected by the disease.
“This study opens up a previously neglected avenue for new disease therapies, for ALS and other neurodegenerative disease,” Roberts said.
Other collaborators on this research include OSU, the University of Melbourne, University of Technology/Sydney, Deakin University, the Australian National University, and the University of Leeds in the United Kingdom.
 Funding has been provided by the Australian National Health and Medical Research Council, the U.S. National Institutes of Health, the Linus Pauling Institute and other groups in Australia and Finland.
Funding has been provided by the Australian National Health and Medical Research Council, the U.S. National Institutes of Health, the Linus Pauling Institute and other groups in Australia and Finland.
###
About the OSU College of Science: As one of the largest academic units at OSU, the College of Science has seven departments and 12 pre-professional programs. It provides the basic science courses essential to the education of every OSU student, builds future leaders in science, and its faculty are international leaders in scientific research.
How Is the Disease Diagnosed?
Lou Gehrig’s disease doesn’t always begin or become worse in the same way. The disease is different for every person who has it. In general, muscle weakness, especially in the arms and legs, is an early symptom for more than half of people with ALS. Other early signs are tripping or falling a lot, dropping things, having difficulty speaking, and cramping or twitching of the muscles. As the disease gets worse over time, eating, swallowing, and even breathing may become difficult.
It may take several months to know for sure that someone has Lou Gehrig’s disease. The illness can cause symptoms similar to other diseases that affect nerves and muscles, including Parkinson’s disease and stroke. A doctor will examine the patient and do special tests to see if it might be one of those other disorders. (It’s like using the process of elimination to figure out the answer to a multiple-choice question on a test.)
One of the tests, an electromyogram (say: eh-lek-tro-MY-uh-gram), or EMG, can show that muscles are not working because of damaged nerves. Other tests include X-rays, magnetic resonance imaging (MRI), a spinal tap, and blood and urine evaluations.
Sometimes a muscle or nerve biopsy is needed. A biopsy is when a doctor takes a tiny sample of tissue from the body to study under a microscope. Examining this tissue can help the doctor figure out what’s making someone sick.
###
Joseph Beckman, 541-737-8867
Oregon State University