Racial/ethnic differences in outcomes following subarachnoid hemorrhage
University of Toronto researchers examined data on patients who had been hospitalized in the United States for subarachnoid hemorrhage (SAH) and found racial/ethnic differences in the rates of inpatient mortality and hospital discharge to institutional care. Compared to white patients, Asian/Pacific Islander patients were more likely and Hispanic patients less likely to die while in the hospital. African-American patients were more likely than white patients to require institutional care following discharge from the hospital, although their risk of death while in the hospital was similar to that of white patients. The likelihood of needing post-hospitalization institutional care was similar among white, Hispanic, Asian/Pacific Islander, and Native American patients. Detailed findings on these racial disparities are reported and discussed in “Racial/ethnic differences in inpatient mortality and use of institutional postacute care following subarachnoid hemorrhage. Clinical article,” by Blessing N. R. Jaja, M.B.B.S., M.Sc., Gustavo Saposnik, M.D., M.Sc., F.R.C.P.C., Rosane Nisenbaum, Ph.D., Benjamin W. Y. Lo, M.D., M.Sc., F.R.C.S.C., Tom A. Schweizer, Ph.D. Kevin E. Thorpe, M.Math., and R. Loch Macdonald, M.D., Ph.D., F.R.C.S., published today online, ahead of print, in the Journal of Neurosurgery.
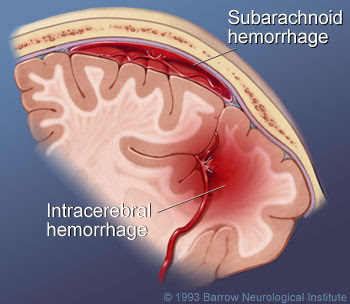
Subarachnoid hemorrhage (SAH) - that is, bleeding into the subarachnoid space that surrounds the brain—can increase pressure in the skull, damage or kill brain cells, and deprive the brain of oxygen. Many victims of SAH do not survive long enough to obtain treatment; those who do may die while undergoing treatment in the hospital, make a complete recovery, or survive with transient or permanent brain defects.
Jaja and colleagues set out to examine whether race or ethnicity had a bearing on who was most likely to die while in the hospital following an SAH and who was most likely to be discharged from the hospital to another post-acute institutional setting for further care. To do so, these researchers performed a cross-sectional study of hospital discharges for patients whose primary diagnosis was SAH unrelated to trauma. They examined data from the Nationwide Inpatient Sample, a large all-payer hospital care database. Focusing on the years 2005 through 2010, the researchers identified 31,631 hospital discharges related to stays for SAH.
In this study, inpatient mortality was the primary outcome and discharge to institutional care was the secondary outcome. In the statistical analyses, the independent variable was patient-identified race/ethnicity: white, black, Hispanic, Asian/Pacific Islander, or Native American. The researchers took into account explanatory or confounding variables in the relationships of race/ethnicity to the primary and secondary outcomes, specifically comorbid conditions as well as demographic, clinical, and hospital-related factors.
Among patients admitted to the hospital for SAH, Jaja and colleagues found a crude inpatient mortality rate of 22% and a 42% rate of hospital discharge to institutional care. Multivariable analyses identified race/ethnicity as a significant predictor of both inpatient mortality (p = 0.003) and discharge to institutional care (p ≤ 0001). In their analyses of the impact of race/ethnicity on the primary and secondary outcomes, the researchers found the following:
Hispanic patients fared best of all racial/ethnic groups. Compared with white patients, Hispanic patients were significantly less likely to die while in the hospital (odds ratio [OR] 0.84), and they shared about the same risk of discharge to institutional care (OR 0.98).
For black patients, the risk of dying in the hospital (OR 1.04) was similar to that for white patients; however, if they survived their hospital stay, black patients had a greater risk of being discharged to institutional care (OR 1.27).
Native American patients were more likely than white patients to die while in the hospital (OR 1.10) or to be transferred to institutional care (OR 1.16) after they left the hospital, but these differences were not statistically significant.
Of all the racial/ethnic groups, Asian/Pacific Islander patients were most likely to die during hospitalization (OR 1.34). They were also more likely than white patients to be discharged to institutional care (OR 1.17), but this difference was not significant.
Based on their findings, the researchers conclude that patients who are admitted to the hospital with SAH differ significantly according to race or ethnicity in both risk of death while in the hospital and risk of needing to be sent to institutional care after discharge from the hospital. Hispanic patients were least likely to have a poor outcome, and Asian Pacific/Islander patients were most likely to have a poor outcome.
 The finding of better outcomes in Hispanic patients was not a surprise to the researchers, although they call it an “epidemiological paradox.” Hispanic persons in the United States on average have a lower socioeconomic status, more risk factors, and less ease of access to medical care than non-Hispanic white persons. Nevertheless, a review of epidemiological studies shows that Hispanic ethnicity is associated with lower risks of death from all causes as well as death due to specific diseases. The researchers mention that investigations are currently focused on this paradox.
The finding of better outcomes in Hispanic patients was not a surprise to the researchers, although they call it an “epidemiological paradox.” Hispanic persons in the United States on average have a lower socioeconomic status, more risk factors, and less ease of access to medical care than non-Hispanic white persons. Nevertheless, a review of epidemiological studies shows that Hispanic ethnicity is associated with lower risks of death from all causes as well as death due to specific diseases. The researchers mention that investigations are currently focused on this paradox.
As to the poor outcomes of Asian/Pacific Islander patients, the authors offer possible causes such as more severe SAH or less access to high-quality hospitals. Here again, further studies are suggested to determine precisely why this group fared worse than the others.
When asked about the study’s message, Dr. R. Loch Macdonald responded, “Blessing [Jaja] and I believe that there could be fundamentally important differences between the biological responses of different ethnic groups to diseases like SAH, rather than any difference due to their medical treatment. If we can understand what the biological basis is for the better outcome of some ethnic groups, then maybe we can develop ways to use the beneficial effects to help everyone with SAH.”
###
 Jaja BNR, Saposnik G, Nisenbaum R, Lo BWY, Schweizer TA, Thorpe KE, Macdonald RL. Racial/ethnic differences in inpatient mortality and use of institutional postacute care following subarachnoid hemorrhage. Clinical article. Journal of Neurosurgery, published online, ahead of print, September 10, 2013; DOI: 10.3171/2013.7.JNS13544
Jaja BNR, Saposnik G, Nisenbaum R, Lo BWY, Schweizer TA, Thorpe KE, Macdonald RL. Racial/ethnic differences in inpatient mortality and use of institutional postacute care following subarachnoid hemorrhage. Clinical article. Journal of Neurosurgery, published online, ahead of print, September 10, 2013; DOI: 10.3171/2013.7.JNS13544
Disclosure: Dr. Saposnik is supported by the Distinguished Clinician Scientist Award from the Heart & Stroke Foundation of Canada (HSFC). He also serves on the editorial boards of Stroke, the Journal of Stroke and Cerebrovascular Disease, and the International Journal of Stroke. Dr. Macdonald discloses the following: ownership of Edge Therapeutics, Inc.; grant support from the Brain Aneurysm Foundation, Physicians Services Incorporated Foundation, HSFC, and the Canadian Institutes of Health Research; and consultant activities for Actelion Pharmaceuticals. This research was not funded by a grant. The authors have no conflict of interest with regard to the methods or materials used in the study or the reported findings.
For additional information, please contact:
Ms. Jo Ann M. Eliason, Communications Manager
Journal of Neurosurgery Publishing Group
One Morton Drive, Suite 200
Charlottesville, VA 22903
Email: .(JavaScript must be enabled to view this email address)
Telephone 434-982-1209
Fax 434-924-2702
###
For 69 years, the Journal of Neurosurgery has been recognized by neurosurgeons and other medical specialists the world over for its authoritative clinical articles, cutting-edge laboratory research papers, renowned case reports, expert technical notes, and more. Each article is rigorously peer reviewed. The Journal of Neurosurgery is published monthly by the JNS Publishing Group, the scholarly journal division of the American Association of Neurological Surgeons. Other peer-reviewed journals published by the JNS Publishing Group each month include Neurosurgical Focus, the Journal of Neurosurgery: Spine, and the Journal of Neurosurgery: Pediatrics.
Founded in 1931 as the Harvey Cushing Society, the American Association of Neurological Surgeons (AANS) is a scientific and educational association with more than 8,300 members worldwide. The AANS is dedicated to advancing the specialty of neurological surgery in order to provide the highest quality of neurosurgical care to the public. All active members of the AANS are certified by the American Board of Neurological Surgery, the Royal College of Physicians and Surgeons (Neurosurgery) of Canada or the Mexican Council of Neurological Surgery, AC. Neurological surgery is the medical specialty concerned with the prevention, diagnosis, treatment and rehabilitation of disorders that affect the entire nervous system including the brain, spinal column, spinal cord, and peripheral nerves.
###
Jo Ann M. Eliason
.(JavaScript must be enabled to view this email address)
434-982-1209
Journal of Neurosurgery Publishing Group