Anti-depressant link to Clostridium difficile infection
Certain types of anti-depressants have been linked to an increase in the risk of Clostridium difficile infection (CDI) finds a study in BioMed Central’s open access journal BMC Medicine. Awareness of this link should improve identification and early treatment of CDI.
CDI is one of the most common hospital acquired infections and is responsible for more than 7000 deaths annually in the USA alone. Several types of medications are thought to increase risk of CDI, including anti-depressants, and given that depression is the third most common medical condition worldwide a team from the University of Michigan investigated the exact nature of this risk.
Firstly the team studied Clostridium difficile infection in people with and without depression and found that people with major depression had a much higher chance of CDI (a 36% increase) than people without depression. This association held for a variety of depressive disorders and nervous or psychiatric problems. Age and family support also impacted risk of CDI. Older, widowed Americans were 54% more likely to catch C. difficile than their married peers. Just living alone increased risk by 25%.
Secondly they looked to see if there was an association between antidepressant medication and hospital acquired CDI. They found that use of most types of antidepressants did not affect CDI risk - out of the twelve drugs tested only mirtazapine and fluoxetine increased risk of CDI, in each case the risk was doubled.
People who have been prescribed these types of anti-depressants need to keep taking them unless otherwise advised by their physician. The researchers stress that it is not yet known whether the increase in CDI is due to microbial changes in the gut during depression or to the medications associated with depression.
Dr. Mary Rogers who led this study explained, “Depression is common worldwide. We have long known that depression is associated with changes in the gastrointestinal system. The interaction between the brain and the gut, called the “brain-gut axis” is fascinating and deserves more study. Our finding of a link between depression and Clostridium difficile should help us better identify those at risk of infection and perhaps, encourage exploration of the underlying brain-gut mechanisms involved.”

Clostridium difficile Infection
People getting medical care can catch serious infections called healthcare-associated infections (HAIs). While most types of HAIs are declining, one – caused by the germ C. difficile – remains at historically high levels. C. difficile causes diarrhea linked to 14,000 American deaths each year. Those most at risk are people, especially older adults, who take antibiotics and also get medical care. CDC provides guidelines and tools to the healthcare community to help prevent Clostridium difficile infections as well as provides resources to help the public safeguard their own health.
###
Media Contact
Dr Hilary Glover
Scientific Press Officer, BioMed Central
Mob: +44 (0) 778 698 1967
What is Clostridium difficile?
Clostridium difficile is a spore-forming, Gram-positive anaerobic bacillus that produces two exotoxins: toxin A and toxin B. It is a common cause of antibiotic-associated diarrhea (AAD). It accounts for 15-25% of all episodes of AAD.
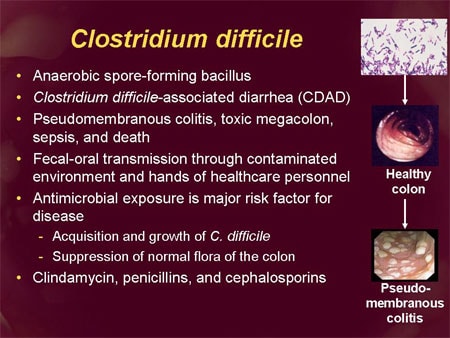
What diseases result from Clostridium difficile infection?
pseudomembranous colitis (PMC)
toxic megacolon
perforations of the colon
sepsis
death (rarely)
What are the main clinical symptoms of Clostridium difficile infection?
Clinical symptoms include:
watery diarrhea
fever
loss of appetite
nausea
abdominal pain/tendernes
Symptoms of a more severe C. diff. infection include:
Frequent, watery diarrhea (up to 15 times each day)
Severe abdominal pain or tenderness
Loss of appetite
Low-grade fever of up to 101°F in children or 100°F to 102°F in adults
Blood or pus in the stool
Which patients are at increased risk for Clostridium difficile infection?
The risk for disease increases in patients with:
antibiotic exposure
proton pump inhibitors
gastrointestinal surgery/manipulation
long length of stay in healthcare settings
a serious underlying illness
immunocompromising conditions
advanced age
Notes to Editors
1. Depression, antidepressant medications, and risk of Clostridium difficile infection Mary A Rogers, M Todd Greene, Vincent B Young, Sanjay Saint, Kenneth M Langa, John Y Kao and David M Aronoff BMC Medicine (in press)
Please name the journal in any story you write. If you are writing for the web, please link to the article. All articles are available free of charge, according to BioMed Central’s open access policy.
2. BMC Medicine is the flagship medical journal of the BMC series, publishing original research, commentaries and reviews that are either of significant interest to all areas of medicine and clinical practice, or provide key translational or clinical advances in a specific field.
3. BioMed Central is an STM (Science, Technology and Medicine) publisher which has pioneered the open access publishing model. All peer-reviewed research articles published by BioMed Central are made immediately and freely accessible online, and are licensed to allow redistribution and reuse. BioMed Central is part of Springer Science+Business Media, a leading global publisher in the STM sector.
###
Hilary Glover
.(JavaScript must be enabled to view this email address)
44-020-319-22370
BioMed Central