Risk of falls increases between cataract surgeries
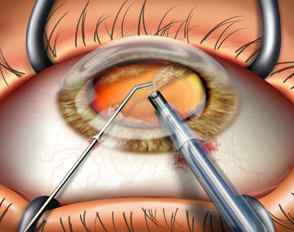
Older adults with cataracts appear to double their risk of falling after surgery on their first eye and before surgery on the second, suggests a new study.
The finding that corrective eye surgery may - at least temporarily - be linked to an increase in falls comes after years of conflicting study results on the subject, researchers write in the journal Age and Ageing.
But the topic remains important as the global population ages and demand for cataract surgery increases. In Australia, where the study was conducted, cataract surgeries tripled over the past two decades.
“This study tells us that timing of cataract surgeries is very important,” Dr. Ediriweera Desapriya of the University of British Columbia in Vancouver, Canada, told Reuters Health.
Desapriya has researched falls in older adults at the Center for Clinical Epidemiological and Evaluation Research, but wasn’t involved in the new study.
“In the past, you didn’t really want to get both eye surgeries done at the same time,” Desapriya said. That was in case of problems like infection or swelling. “But now the technology has improved and complications occur less often,” he said.
 For their study, Lynn Meuleners of Curtin University and her team in Perth looked back through detailed electronic health records from Western Australia’s hospitals and its death registry.
For their study, Lynn Meuleners of Curtin University and her team in Perth looked back through detailed electronic health records from Western Australia’s hospitals and its death registry.
Between 2001 and 2008, nearly 28,400 older adults in the region had cataract surgery on both eyes. The researchers found 1,094 of them also took a fall serious enough to warrant a hospital visit during that period.
People waited an average of 10 months between eye surgeries. Compared to the two-year period before any cataract surgery, their chance of falling doubled between procedures.
In the two years after surgery on their second eye, people’s fall risk was 34 percent higher than before their first surgery. The risk of falling also rose with age.
Most people who fell were older than 80, women, city dwellers and were not married.
“It’s a well-conducted study,” said Stephen Lord, a senior principal research fellow with Neuroscience Research Australia in Sydney. Lord was not involved with the current study, but researches balance and falls among older adults.
“In the intervening time between surgeries, you have a person with two eyes that are no longer equal and this can lead to various effects,” Lord said - like on visual sharpness and depth of field.
“For these things, we need two eyes working together,” he told Reuters Health.
However, at least one previous randomized controlled trial - medicine’s gold standard for research - found people had fewer falls after cataract surgery, Lord said.
Based on this study, doctors could warn patients to be extra cautious after having surgery on their first eye, Desapriya said.
“It is also important to encourage patients to have a second eye cataract surgery early,” Desapriya said. “Otherwise, eyes continue to function monocularly (with just one eye) and patients lose their depth perception.”
The new research cannot point to cataract surgery as the primary cause of the falls - it only suggests they are linked.
The researchers said a limitation of their study is a lack of knowledge about people’s lifestyles, including their living situations, and co-existing eye conditions, both of which could strongly influence fall risk.
They also did not look at falls among people who had not undergone cataract surgery. Such comparisons are helpful when considering changes in risk.
“The aging population is growing rapidly in the U.S. and Canada,” Desapriya said. “And this surgery is becoming a very common clinical procedure.”
According to the National Eye Institute, more than half of all Americans have a cataract or have had cataract surgery by the time they’re 80.
Lord compared cataract surgery to a major change in prescription eyeglasses: in both cases, the brain needs time to adjust to the changes in vision.
But patients and doctors should not shy away from cataract operations, Lord said.
“The last thing we want to have happen is to prevent people from receiving cataract surgery,” Lord said. “This surgery has many benefits, such as improving quality of life, increasing a person’s participation in the community and even preventing falls in the longer term.”
“It just seems that, in the short term, there may be a problem while people adjust to their new vision,” he said.
SOURCE: Age and Ageing, online November 4, 2013
###
The impact of first- and second-eye cataract surgery on injurious falls that require hospitalisation: a whole-population study
Results: the risk of an injurious fall that required hospitalisation doubled (risk ratio: 2.14, 95% confidence interval: 1.82 to 2.51) between first- and second-eye cataract surgery compared with the 2 years before first-eye surgery. There was a 34% increase in the number of injurious falls that required hospitalisation in the 2 years after second-eye cataract surgery compared with the 2 years before first-eye surgery (risk ratio: 1.34, 95% confidence interval: 1.16–1.55).
Conclusions: there was an increased risk of injurious falls after first- and second-eye cataract surgery which has implications for the timely provision of second-eye surgery as well as appropriate refractive management between surgeries.
Lynn B. Meuleners,
Michelle Louise Fraser,
Jonathan Ng and
Nigel Morlet