Research reveals possible cause of diabetic cardiomyopathy
Researchers from the University of Texas Medical Branch at Galveston have discovered one of the pathogenic components of diabetes in the heart, as published in the Journal of Biological Chemistry.
While both heart disease and diabetes are widely studied, how diabetic cardiomyopathy develops is not well understood, other than that it seemed to be linked to protein kinase C (PKC) — a family of enzymes that controls the functions of other proteins by using phosphates to turn them on and off.
Researchers at UTMB, led by assistant professor of biochemistry Dr. Muge Kuyumcu-Martinez, studied the effects of PKC signals in the hearts of diabetic mice.
“We now know that the leading cause of diabetic cardiomyopathy can be attributed to PKC activation and its downstream effects on gene expression,” said Kuyumcu-Martinez. “Knowing how cardiomyopathy manifests, further research can use these results to concentrate on the prevention and treatment of heart failure in diabetics.”
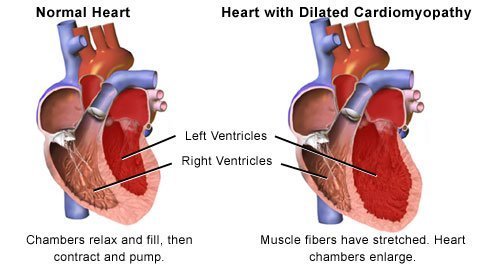
Cardiomyopathy, a known symptom of diabetes, occurs when the muscles of the heart weaken, and the heart is no longer strong enough to pump blood and properly circulate it throughout the body. Adults with diabetes are two to four times more likely to die of heart failure than the rest of the population.
 The researchers discovered that when PKC is over-activated, the cells of the adult heart revert to splicing methods used during the embryonic stages. Genes contain codes for certain processes and products, such as proteins, and they send signals to the body to complete these processes and products through messenger RNA. Alternative splicing occurs when one gene contains the codes for multiple proteins. The human genome contains 20,000 protein-coding genes, so using one gene to create more than one protein is an efficient process - when it’s running correctly. But problems occur when the genetic information is abnormally spliced or mis-spliced to messenger RNA, giving it mutated instructions. As much as one-third of genetic disease and many cancers are attributed to splicing changes.
The researchers discovered that when PKC is over-activated, the cells of the adult heart revert to splicing methods used during the embryonic stages. Genes contain codes for certain processes and products, such as proteins, and they send signals to the body to complete these processes and products through messenger RNA. Alternative splicing occurs when one gene contains the codes for multiple proteins. The human genome contains 20,000 protein-coding genes, so using one gene to create more than one protein is an efficient process - when it’s running correctly. But problems occur when the genetic information is abnormally spliced or mis-spliced to messenger RNA, giving it mutated instructions. As much as one-third of genetic disease and many cancers are attributed to splicing changes.
In the case of diabetic cardiomyopathy, the research team used RNA sequencing technology to identify 22 specific alternative splicing events that occur, causing a developmental shift in the gene expression. This shift causes mechanisms of the heart to behave as though it were still an embryo, which prevents the heart from functioning correctly in a full-grown adult fighting diabetes.
Diabetic Cardiomyopathy
It has been over 30 years since Rubler et al. described four diabetic patients with congestive heart failure (CHF), normal coronary arteries, and no other etiologies for CHF and proposed that it was due to diabetic cardiomyopathy. Eight years ago, I reviewed the evidence for diabetic cardiomyopathy as a unique entity unassociated with coronary artery disease and concluded that diabetic cardiomyopathy was a distinct entity characterized by diastolic dysfunction, which was rarely clinically apparent unless associated with hypertension (when it was likely to become clinically apparent) and/or with myocardial ischemia (when it was likely to present with severe clinical manifestations). At that time the evidence also suggested that diastolic dysfunction was due to myocellular hypertrophy and myocardial fibrosis, and at the cellular level there were defects in calcium transportation, myocardial contractile protein collagen formation, and fatty acid metabolism . Since then we have learned that diabetic cardiomyopathy is not a rare condition but instead a very common one, and that its etiology is largely due to hyperglycemia with contributions from the insulin resistance syndrome that cause left ventricular hypertrophy.
Left ventricular diastolic dysfunction is characterized by impairment in early diastolic filling, prolongation of isovolumetric relaxation, and increased atrial filling, and these characteristics have even been documented in young type 1 diabetic patients. Older studies of well-controlled type 2 diabetic subjects showed that 30% had diastolic dysfunction. However, this prevalence was based on standard echocardiography testing, in which mild and early diastolic dysfunction is not detectable in approximately one-third of subjects. When more rigorous Doppler methods are used, early and mild diastolic dysfunction can be diagnosed. Using these methods in Olmstead County, Minnesota, 52% of diabetic subjects were shown to have diastolic dysfunction. Using similarly sensitive methods, Porier et al. showed the prevalence of diastolic dysfunction to be 60% in well-controlled type 2 diabetic patients. Therefore, it is not surprising that in this issue of Diabetes Care, Bertoni et al. have documented that the diagnosis of idiopathic cardiomyopathy is more common in the diabetic patient.
 While these studies of diastolic dysfunction were performed in diabetic patients with a normal left ventricular mass, left ventricular hypertrophy is more prevalent in type 2 diabetic patients and contributes to ventricular dysfunction. In the Framingham Heart study, diabetic women had a left ventricular mass 10% greater than that of their nondiabetic peers; and in the Tayside Study, left ventricular hypertrophy was present in 32% of normotensive type 2 diabetic subjects who were not utilizing ACE inhibitors and had no known coronary artery disease. Unlike myocardial fibrosis, which is likely due to hyperglycemia, left ventricular hypertrophy is most likely related to the insulin resistance syndrome .
While these studies of diastolic dysfunction were performed in diabetic patients with a normal left ventricular mass, left ventricular hypertrophy is more prevalent in type 2 diabetic patients and contributes to ventricular dysfunction. In the Framingham Heart study, diabetic women had a left ventricular mass 10% greater than that of their nondiabetic peers; and in the Tayside Study, left ventricular hypertrophy was present in 32% of normotensive type 2 diabetic subjects who were not utilizing ACE inhibitors and had no known coronary artery disease. Unlike myocardial fibrosis, which is likely due to hyperglycemia, left ventricular hypertrophy is most likely related to the insulin resistance syndrome .
David S.H. Bell, MB, FACE
Author Affiliations
From the University of Alabama School of Medicine, Birmingham, Alabama
Address correspondence to David S.H. Bell, MB, FACE, Faculty Office Tower, Room 702, 510 South 20th St., Birmingham, AL 35294-3407. E-mail: .(JavaScript must be enabled to view this email address)
###
Other members of this research team from UTMB’s department of biochemistry and molecular biology included postdoctoral fellow Sunil K. Verma, research associate Vaibhav Deshmukh, graduate assistant Curtis A. Nutter, and research associate Rosario Espejo. Patrick Liu and Gene W. Yeo of the University of California, San Diego and Ming-Lung Hung and Guey-Shin Wang of Academia Sinica in Taipei also contributed.
Funding for the study was provided by the UTMB department of biochemistry and molecular biology, the American Heart Association, the March of Dimes Foundation and the National Institutes of Health. This work was partly supported by the National Science Council, Taiwan and the Institute of Biomedical Sciences, Academia Sinica.
###
Kristen Hensley
.(JavaScript must be enabled to view this email address)
409-772-8772
University of Texas Medical Branch at Galveston