Health Centers > Obesity and Weight Management Health Center > Childhood obesity
Childhood obesity
Worldwide prevalence of childhood obesity has increased greatly during the past three decades. The increasing occurrence in children of disorders such as type 2 diabetes is believed to be a consequence of this obesity epidemic.
Childhood obesity
Childhood obesity is a serious medical condition that affects children and adolescents. It occurs when a child is well above the normal weight for his or her age and height.
Childhood obesity is particularly troubling because the extra pounds often start children on the path to health problems that were once confined to adults, such as diabetes, high blood pressure and high cholesterol. Childhood obesity can also lead to poor self-esteem and depression.
One of the best strategies to reduce childhood obesity is to improve the diet and exercise habits of your entire family. Treating and preventing childhood obesity helps protect the health of your child now and in the future.
Much progress has been made in understanding of the genetics and physiology of appetite control and from these advances, elucidation of the causes of some rare obesity syndromes. However, these rare disorders have so far taught us few lessons about prevention or reversal of obesity in most children. Calorie intake and activity recommendations need reassessment and improved quantification at a population level because of sedentary lifestyles of children nowadays.
For individual treatment, currently recommended calorie prescriptions might be too conservative in view of evolving insight into the so-called energy gap. Although quality of research into both prevention and treatment has improved, high-quality multicentre trials with long-term follow-up are needed. Meanwhile, prevention and treatment approaches to increase energy expenditure and decrease intake should continue. Recent data suggest that the spiralling increase in childhood obesity prevalence might be abating; increased efforts should be made on all fronts to continue this potentially exciting trend.
Epidemiology
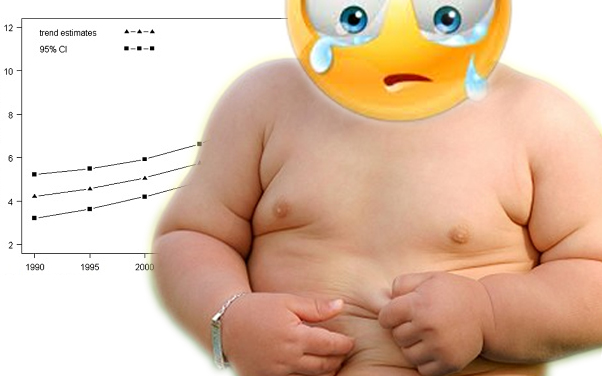
8 years have passed since the last Seminar on childhood obesity in The Lancet.1 Our goal is to review new information and outline some of the remaining challenges. A review of secular trends in the number of overweight or obese children concluded that prevalence had increased during the past two to three decades in most industrialised countries, apart from Russia and Poland, and in several low-income countries, especially in urban areas.2
Prevalence doubled or trebled between the early 1970s and late 1990s in Australia, Brazil, Canada, Chile, Finland, France, Germany, Greece, Japan, the UK, and the USA.2 By 2010, more than 40% of children in the North American and eastern Mediterranean WHO regions, 38% in Europe, 27% in the western Pacific, and 22% in southeast Asia were predicted to be overweight or obese. However, that 2006 review pre-dates recent data, which, although still too soon to be certain, suggest that the increase in childhood obesity in the USA, the UK, and Sweden might be abating.3-5
Internationally agreed thresholds of body-mass index (BMI) define underweight, normal weight, overweight, and obesity in adults, but in children, effects of age, sex, puberty, and race or ethnicity on growth make classification dificult. Definition of a standard age-related growth chart and clinically meaningful thresholds for overweight and obesity present challenges. The International Obesity Taskforce (IOTF) international standard growth chart enables global comparison of prevalence.6 However, many countries continue to use their own country-specific charts, including the USA, where standards are based on a national survey from the early 1960s, before the present epidemic.7
Widely used thresholds for being overweight or obese in childhood are: 110% or 120% of ideal weight for height; weight-for-height Z scores of higher than 1 or higher than 2, and BMI at the 85th, 90th, 95th, and 97th percentiles (on the basis of international or country-specific reference populations).2 The IOTF recommend using their international growth charts and limits specific to age and sex that, on average, correspond to adult thresholds. The IOTF classification has high specificity, but low sensitivity.8
Childhood Obesity Facts
Childhood obesity has more than doubled in children and quadrupled in adolescents in the past 30 years.
The percentage of children aged 6 - 11 years in the United States who were obese increased from 7% in 1980 to nearly 18% in 2012. Similarly, the percentage of adolescents aged 12 - 19 years who were obese increased from 5% to nearly 21% over the same period.
In 2012, more than one third of children and adolescents were overweight or obese.
Overweight is defined as having excess body weight for a particular height from fat, muscle, bone, water, or a combination of these factors.3 Obesity is defined as having excess body fat.
Overweight and obesity are the result of "caloric imbalance" - too few calories expended for the amount of calories consumed - and are affected by various genetic, behavioral, and environmental factors.
Determinants and risk factors
A historical convergence of forces, biological and technological, has led to the obesity epidemic. During millennia of frequent food scarcities, natural selection probably favoured people with parsimonious energy metabolism, known as the thrifty gene hypothesis.9
Although the advent of agriculture about 14 000 years ago ensured more stable food supplies, activities of daily living still needed substantial energy expenditure until about 50 years ago, when radical changes occurred in food availability and energy expenditure. The obesity epidemic is probably the result of evolutionary legacy interacting with our technologically advanced and consumerist society.
Population groups in North America who have preserved traditional lifestyles with substantial embedded physical activity have reduced prevalences of obesity.10 Likewise, in countries with low and middle incomes, the obesity epidemic is largely occurring in urban areas that have easy access to energy-dense cheap foods and low energy requirements in daily life.2
Obesity is a complex disorder that is affected by many interacting genetic and non-genetic factors. We focus mainly on prevention and treatment.
Search strategy and selection criteria
We identified original research, reviews, and commentaries by searching PubMed using the search terms "paediatric obesity", "childhood obesity", "paediatric overweight", "childhood overweight", and "body mass index in children". All dates and languages were considered. Articles published between 1962 and 2010 were included, but we directed special attention to reports published since 2002. Research developments and published work were also identified by discussions with specialists in paediatric obesity, nutrition, and public health.
The table summarises determinants or risk factors that are associated with childhood obesity or variation in adiposity, and figure 1 shows a simplified model of leptin signalling, which is the key biological pathway controlling energy balance.2,4,11-45
 Figure 1: A simplified model of the leptin signalling pathway
Lines with arrowheads show stimulatory action. Lines with perpendicular endblocks show inhibitory action. AgRP=agouti-related protein. BDNF=brain-derived neurotrophic factor. CART=cocaine-amphetamine related transcript. CPE=carboxypeptidase E. CRH=corticotropin-releasing hormone. GABA=gamma amino butyric acid.
Figure 1: A simplified model of the leptin signalling pathway
Lines with arrowheads show stimulatory action. Lines with perpendicular endblocks show inhibitory action. AgRP=agouti-related protein. BDNF=brain-derived neurotrophic factor. CART=cocaine-amphetamine related transcript. CPE=carboxypeptidase E. CRH=corticotropin-releasing hormone. GABA=gamma amino butyric acid.
GI=gastrointestinal. IR=insulin receptor. LR=leptin receptor. MCH=melanin-concentrating hormone. MSH=melanocyte-stimulating hormone. NPY=neuropeptide Y.
PC1=prohormone convertase 1. POMC=pro-opiomelanocortin. PYY=peptide YY. TRH=thyrotropin-releasing hormone. TrkB=tropomyosin receptor kinase B.
Childhood obesity has both immediate and long-term effects on health and well-being.
Immediate health effects:
Obese youth are more likely to have risk factors for cardiovascular disease, such as high cholesterol or high blood pressure. In a population-based sample of 5- to 17-year-olds, 70% of obese youth had at least one risk factor for cardiovascular disease.
Obese adolescents are more likely to have prediabetes, a condition in which blood glucose levels indicate a high risk for development of diabetes.
Children and adolescents who are obese are at greater risk for bone and joint problems, sleep apnea, and social and psychological problems such as stigmatization and poor self-esteem. Long-term health effects:
Children and adolescents who are obese are likely to be obese as adults and are therefore more at risk for adult health problems such as heart disease, type 2 diabetes, stroke, several types of cancer, and osteoarthritis. One study showed that children who became obese as early as age 2 were more likely to be obese as adults.
Overweight and obesity are associated with increased risk for many types of cancer, including cancer of the breast, colon, endometrium, esophagus, kidney, pancreas, gall bladder, thyroid, ovary, cervix, and prostate, as well as multiple myeloma and Hodgkin's lymphoma.
Determinants or risk factors for development of childhood Obesity or increased adiposity
Since the discovery of leptin, understanding of the mechanisms controlling energy balance has rapidly advanced. Apart from leptin replacement therapy in a few leptin-deficient individuals, interventions that effectively prevent or treat obesity in the general population are yet to emerge. Both insulin and leptin are secreted in proportion to body fat and serve as adiposity signals, acting on the same neurons of the hypothalamic arcuate nucleus to regulate energy homoeostasis. Ghrelin, which is secreted by the stomach and duodenum, serves as a hunger signal at the hypothalamus and brainstem, whereas other peptides secreted by the gastrointestinal tract, including peptide YY, act as satiation signals.
The ligands leptin,46 pro-opiomelanocortin,47,48 cocaine-amphetamine related transcript,49 and brain-derived neurotrophic factor (BDNF),16,50 the receptors for leptin,51,52 melanocortins,53-56 and BDNF,57 and the enzyme prohormone convertase 158,59 have function-changing mutations that are associated with obesity in children. Mutations in the ligands and receptors for neuropeptide Y,60 agouti-related protein,61 carboxypeptidase E,62,63 and melanin-concentrating hormome64 change energy balance in rodents, but have not been convincingly associated with human obesity. For several risk factors, evidence is weak and, although important advances have been made, how to incorporate the information effectively and cost-effectively into prevention programmes for children is unclear.
Joan C Han, Debbie A Lawlor, Sue Y S Kimm
Lancet 2010; 375: 1737-48
Published Online May 6, 2010 DOI:10.1016/ S0140- 6736(10)60171-7
Unit on Growth and Obesity, Program on Developmental Endocrinology and Genetics, Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health, DHHS, Bethesda, MD, USA (J C Han MD); MRC Centre for Causal Analyses in Translational Epidemiology, Department of Social Medicine, University of Bristol, Bristol, UK (Prof D A Lawlor PhD); and Department of Internal Medicine/Epidemiology, University of New Mexico School of Medicine, Albuquerque, NM, USA (S Y S Kimm MD)
Correspondence to: Dr Sue Y S Kimm, University of New Mexico Health Sciences Center, Department of Internal Medicine/Epidemiology, University of New Mexico, MSC 10 5550 Albuquerque, NM 87131-0001, USA kimm@pitt.edu
###
REFERENCES
Full References »