Gastric bypass surgery lowers women’s alcohol tolerance
Women who have gastric bypass surgery to lose weight should keep a close eye on their alcohol consumption, according to new research at Washington University School of Medicine in St. Louis.
A small study indicates that changes in how alcohol is metabolized after surgery can speed its delivery into the bloodstream, resulting in earlier and higher peaks in blood-alcohol levels. Studying women who had undergone gastric bypass surgery, the researchers found that those who had consumed the equivalent of two drinks in a short period of time had blood-alcohol contents similar to women who had consumed four drinks but had not had the operation.
The research is published Aug. 5 in the journal JAMA Surgery.
“The findings tell us we need to warn patients who have gastric bypass surgery that they will experience changes in the way their bodies metabolize alcohol,” said first author M. Yanina Pepino, PhD, an assistant professor of medicine in the Division of Geriatrics and Nutritional Science. “Consuming alcohol after surgery could put patients at risk for potentially serious problems, even if they consume only moderate amounts of alcohol.”
Although this study included only women, it is likely that men who have gastric bypass surgery experience similar changes in how their bodies metabolize alcohol.
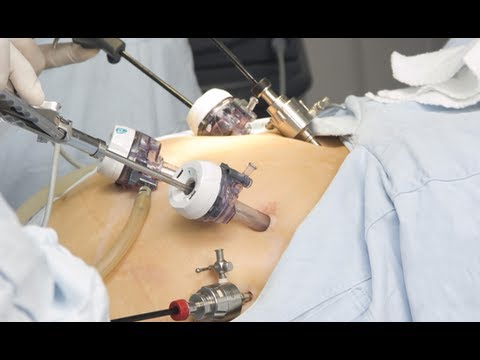 The researchers studied alcohol’s effects in 17 obese women. Eight of the women had undergone Roux-en-Y gastric bypass surgery - the most common bariatric surgical procedure worldwide - one to five years before the study began. The other nine participants had not yet had the operation.
The researchers studied alcohol’s effects in 17 obese women. Eight of the women had undergone Roux-en-Y gastric bypass surgery - the most common bariatric surgical procedure worldwide - one to five years before the study began. The other nine participants had not yet had the operation.
Gastric bypass surgery
Gastric bypass is surgery that helps you lose weight by changing how your stomach and small intestine handle the food you eat.
After the surgery, your stomach will be smaller. You will feel full with less food.
The food you eat will no longer go into some parts of your stomach and small intestine that absorb food. Because of this, your body will not get all of the calories from the food you eat.
As part of the study, the women spent two days, about one week apart, at Washington University’s Clinical Research Center. On one visit, each woman randomly consumed either the equivalent of two alcoholic drinks or two nonalcoholic beverages during a 10-minute period. At the second visit, each was given the beverages not received during the first visit. At both visits, the researchers measured the women’s blood-alcohol contents and used a survey to assess their feelings of drunkenness.
The women in the gastric bypass group had an average body mass index (BMI) of 30, which is considered obese, but it compared with an average BMI of 44 for the women who had not yet had the surgery. Among those who had not undergone surgery, blood-alcohol content peaked about 25 minutes after they finished consuming the alcohol and measured 0.60. In women who had the surgery, blood-alcohol content peaked at 5 minutes after drinking and reached 1.10, significantly above the legal driving limit of 0.80.
“These findings have important public safety and clinical implications,” said senior investigator Samuel Klein, MD, the William H. Danforth Professor of Medicine and director of the Center for Human Nutrition. “After just two drinks, the blood-alcohol content in the surgery group exceeded the legal driving limit for 30 minutes, but the levels in the other group never reached the legal limit.
“The peak blood-alcohol content in the surgery group also met the criteria that the National Institute on Alcohol Abuse and Alcoholism uses to define an episode of binge drinking, which is a risk factor for developing alcohol problems.”
Women who had undergone gastric bypass also reported feeling the effects of alcohol earlier and for longer periods of time than women who had not had the surgery.
The study is not the first to find that gastric bypass surgery can alter alcohol metabolism, but Pepino said it is significant because earlier studies had measured blood alcohol less vigorously and were less clear about the extent of the changes in alcohol metabolism.
“The women who had the surgery only received the equivalent of two drinks, but it was as if they had consumed twice that amount,” she said. “Consuming alcohol after surgery the way one did before the operation could put patients at risk for potentially serious consequences, even when they drink only moderate amounts of alcohol.”
###
Funding for the research comes from the National Institute on Alcohol Abuse and Alcoholism, the National Institute of Diabetes and Digestive and Kidney Diseases and the National Center for Research Resources of the National Institutes of Health (NIH), grant numbers AA 020018, DK 56341, UL1 RR024992 and AA 11998; and by the Midwest Alcohol Research Center.
Pepino MY, Okunade AL, Eagon JC, Bartholow BD, Bucholz K, Klein S. Effect of Roux-ex-Y gastric bypass surgery: converting 2 alcoholic drinks to 4. JAMA Surgery, published online Aug. 5, 2015. doi:10.1001/jamasurg.2015.1884
Washington University School of Medicine’s 2,100 employed and volunteer faculty physicians also are the medical staff of Barnes-Jewish and St. Louis Children’s hospitals. The School of Medicine is one of the leading medical research, teaching and patient-care institutions in the nation, currently ranked sixth in the nation by U.S. News & World Report. Through its affiliations with Barnes-Jewish and St. Louis Children’s hospitals, the School of Medicine is linked to BJC HealthCare.
###
Jim Dryden
.(JavaScript must be enabled to view this email address)
314-286-011