Bariatric surgery not a magic wand to curb depression
Most severely obese people experience much better spirits once they shed weight through a diet, lifestyle changes or medical intervention. This is unfortunately not true for everyone, says Valentina Ivezaj and Carlos Grilo of the Yale University School of Medicine in the US. In an article in Springer’s journal Obesity Surgery, the researchers advise that the levels of depression in patients be measured six to 12 months after they have had such bariatric surgery. This will ensure that the necessary help can be provided when needed.
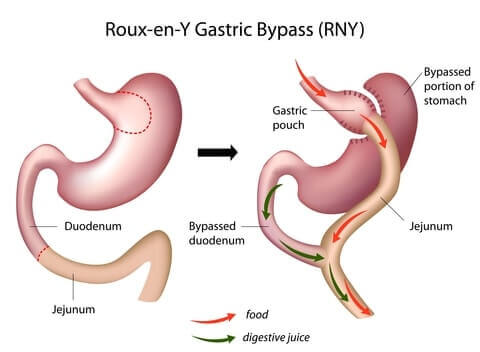
Ivezaj and Grilo set out to investigate how prone bariatric patients are to still experiencing depressive symptoms, and especially if such symptoms increase markedly or not at all, after post-surgery. Their study is the first to examine patients with discernible worsening depressive symptoms six and 12 months following gastric bypass surgery.
Self-reported questionnaires were completed by 107 patients with extreme obesity before they underwent gastric bypass surgery, and then again six and 12 months after the procedure. They were asked to reflect on their levels of depression, possible eating disorders, their self-esteem and general social functioning. Of the 107 participants, 94 were women and 13 were men, 73 were white and 24 had completed college.
Consistent with previous research, Ivezaj and Grilo observed that most people who had undergone this procedure were in much better spirits. In fact, most patients reported experiencing a normal and improved mood at six and 12 months after surgery. However, in some cases negative mood changes started to creep in between six and 12 months after the operation, with 3.7 percent of patients reporting that they felt discernibly more depressed 12 months post-surgery. Between six and 12 months after the operation, however, even more patients (13.1 percent) reported increases in depressive symptoms. These changes went hand-in-hand with significantly lower levels of self-esteem and social functioning.
“The majority of patients whose mood had worsened discernibly experienced these mood changes between six and 12 months post-surgery, suggesting this may be a critical period for early detection and intervention, as needed,” explains Ivezaj.
“The increases in symptoms of depression are also notable given that they were associated with other difficulties including lower self-esteem and social functioning,” adds Grilo.
Depression after Bariatric Surgery: Triggers, Identification, Treatment, and Prevention
A recent study in the Archives of Surgery has caught the attention of the bariatric community. It found the suicide rate after bariatric surgery to be at least five times that of the general population.1 This study may be thought of as important preliminary information, but it does not yet adequately explain the relationship between suicide and bariatric surgery. Nevertheless, this new information does highlight a need for bariatric professionals to educate their patients as to the possibility of depression postoperatively.
Psychological Triggers for Depression
“Why would I be depressed when I’m losing weight?”
This is a common response from patients when I discuss the possibility of depression after surgery. Most people approach the surgery with a positive attitude. Thoughts about future weight reduction, health benefits, and improved quality of life are dominant while awaiting surgery. After surgery however, reality does not always live up to the preoperative fantasy, and some patients do experience depression.2 In general, bariatric patients report a higher rate of depression than the non-bariatric population.3 One study found that of preoperative patients with no depression, over one-third of the sample developed depression postoperatively.4
“If I’m losing weight I won’t miss the food.”
This is a commonly held but unrealistic hope. Food not only nourishes our bodies, but it also serves other purposes. Food is present in almost every one of our societal ceremonies. From weddings to funerals, we eat to celebrate and to mourn. Socialization revolves around food as well. Going out to dinner is a popular activity with friends. Almost every major holiday is enhanced with a traditional menu. Postoperative patients often find themselves feeling as though they are on the outside of things. They realize that life goes on as usual, but they cannot participate in a ritual in the same way. This initial realization and subsequent mild depression may be conceptualized as the normal postoperative blues. It is not uncommon to hear, “What was I thinking when I decided to do this?” Many patients tell me they are “mourning the loss of food as a friend.” In my practice, I have observed many patients go through this, but most feel better within 2 to 3 months.
“When I can’t eat after surgery, I’ll lose weight, and then I just won’t go back to my old habits.”
This too is an unrealistic hope for many. It is normal for people to use food to deal with emotions. Some people use it to compensate for a bad day, others to celebrate, and still others to calm anxiety or depression. The tendency to eat for these reasons does not appear to change, although there is a period of a year or two when these cravings and urges may diminish. They do, however, almost always return. Eating disturbances before surgery tend to predict eating disturbances postoperatively following a short dormant period.5 In my groups I see a subset of people dealing with the reality that the surgery does not do all the work, and these postoperative patients are struggling once again to control emotional eating. This realization can lead to feelings of depression. Weight regain may occur during this time, further exacerbating the depression.
 The authors note that the increases in depressive symptoms were indicative of only subthreshold or mild mood disturbances. They also indicated that future research is needed to determine whether these mood changes continue to worsen over time for this group.
The authors note that the increases in depressive symptoms were indicative of only subthreshold or mild mood disturbances. They also indicated that future research is needed to determine whether these mood changes continue to worsen over time for this group.
Reference:
Ivezaj, V. & Grilo, C.M. (2014). When Mood Worsens after Gastric Bypass Surgery: Characterization of Bariatric Patients with Increases in Depressive Symptoms Following Surgery, Obesity Surgery DOI 10.1007/s11695-014-1402-z.
Depression No Barrier to Weight-Loss Surgery
New research shows that depression and anxiety are common in morbidly obese patients undergoing bariatric surgery, but this doesn’t seem to interfere with the success of the surgery. In fact, having the surgery might ease depressive symptoms.
Jonathan F. Finks, MD, assistant professor of surgery at the University of Michigan in Ann Arbor, reported the findings at the American Society for Metabolic and Bariatric Surgery (ASMBS) 28th Annual Meeting in Orlando, Florida.
“How prevalent depression is in the bariatric population and whether having a psychiatric disease affects bariatric surgery outcomes is not very well known,” he noted in an interview with Medscape Medical News. “What effect bariatric surgery may have on psychiatric outcomes is also not that well known.”
To investigate, Dr. Finks and colleagues examined data on patients enrolled in the Michigan Bariatric Surgery Collaborative, a prospective clinical registry of bariatric surgery patients in the state.
Among the 25,469 patients who underwent bariatric surgery between 2006 and 2010, 11,687 (46%) were being treated for at least 1 psychiatric disorder. The most common were depression (41%) and anxiety (15%). Follow-up surveys of these patients were conducted each year for 3 years after surgery.
###
Springer, Part of Springer Science+Business Media