No evidence of long-term PTSD risk in patients with awareness during surgery
Patients with confirmed episodes of awareness during anesthesia and surgery don’t seem to be at increased risk of posttraumatic stress disorder (PTSD) or other problems with psychosocial well-being at long-term follow-up, reports a study in Anesthesia & Analgesia.
“We found no indication that intraoperative awareness with recall had any long-term effects on patients’ psychosocial outcome,” concludes the new research by Dr Tanja Laukkala of the Centre for Military Medicine in Helsinki, Finland. Anesthesiologists “should respond to the findings…with a mixture of cautious optimism coupled with a renewed commitment to the prevention and treatment of PTSD” after intraoperative awareness, according to an editorial by Dr George A. Mashour of University of Michigan Medical School and Dr Michael S. Avidan of Washington University, St Louis.
No Long-Term Cases of PTSD after Awareness during Anesthesia The long-term follow-up study included nine patients with a documented episode of intraoperative awareness during general anesthesia. All patients had “definite awareness with recall” - they accurately described events that occurred during their surgery. The patients were identified from previous Finnish studies of intraoperative awareness.
A median of 17.2 years after their episode of intraoperative awareness, the patients were evaluated on a battery of tests of psychosocial well-being. Assessment included formal diagnostic interviews for PTSD, along with anxiety, depression, and other psychiatric disorders. Nine patients with similar characteristics - who had undergone surgery without intraoperative awareness - were studied for comparison.
The results showed no significant difference in psychosocial outcomes for the patients with versus without intraoperative awareness. In particular, none of the patients with intraoperative awareness were diagnosed with PTSD.
In fact, in no patient did the episode of intraoperative awareness meet criteria for being a “potentially traumatic event” of the type leading to PTSD. Other measures of psychosocial well-being, including quality of life ratings, were also similar between groups. A few patients in each group had depression or other psychiatric disorders.
Post-traumatic stress disorder (PTSD) is a mental health condition that’s triggered by a terrifying event - either experiencing it or witnessing it. Symptoms may include flashbacks, nightmares and severe anxiety, as well as uncontrollable thoughts about the event.
Many people who go through traumatic events have difficulty adjusting and coping for a while, but they don’t have PTSD - with time and good self-care, they usually get better. But if the symptoms get worse or last for months or even years and interfere with your functioning, you may have PTSD.
Getting effective treatment after PTSD symptoms develop can be critical to reduce symptoms and improve function.
 Ongoing Efforts Needed to Prevent Intraoperative Awareness Intraoperative awareness with recall is an uncommon but documented complication in patients undergoing general anesthesia. Previous studies have suggested that intraoperative awareness may place patients at risk for PTSD and other mental health conditions, such as depression or alcohol abuse. Because intraoperative awareness is rare, it is difficult to study the possible psychological after-effects.
Ongoing Efforts Needed to Prevent Intraoperative Awareness Intraoperative awareness with recall is an uncommon but documented complication in patients undergoing general anesthesia. Previous studies have suggested that intraoperative awareness may place patients at risk for PTSD and other mental health conditions, such as depression or alcohol abuse. Because intraoperative awareness is rare, it is difficult to study the possible psychological after-effects.
Previous studies have reported high rates of PTSD after intraoperative awareness, but have had important limitations. For example, some studies have recruited patients through advertising, introducing a potential source of bias.
The new report is the longest follow-up study of patients with documented episodes of intraoperative awareness with recall. Dr Laukkala and coauthors note that the patients in their study received “appropriate psychosocial support and services” and explanations of their memories and symptoms—which may have lessened the long-term impact of the event.
Who gets PTSD?
Anyone can get PTSD at any age. This includes war veterans and survivors of physical and sexual assault, abuse, accidents, disasters, and many other serious events.
Not everyone with PTSD has been through a dangerous event. Some people get PTSD after a friend or family member experiences danger or is harmed. The sudden, unexpected death of a loved one can also cause PTSD.
The results suggest that intraoperative awareness doesn’t necessarily increase the risk of PTSD and other mental health problems. The researchers write, “We emphasize that it is of utmost importance to try to prevent intraoperative awareness, and when recognized, potentially traumatized individuals should be offered support according to evidence-based guidelines.”
While the findings are reassuring, they do not mean there’s no risk of PTSD after an episode of intraoperative awareness, according to Drs Mashour and Avidan. In their editorial, they call for further studies to understand which procedures or patients are associated with a higher risk of intraoperative awareness and PTSD, to facilitate early recognition and prompt treatment.
How is PTSD detected?
A doctor who has experience helping people with mental illnesses, such as a psychiatrist or psychologist, can diagnose PTSD. The diagnosis is made after the doctor talks with the person who has symptoms of PTSD.
To be diagnosed with PTSD, a person must have all of the following for at least 1 month:
At least one re-experiencing symptom
At least three avoidance symptoms
At least two hyperarousal symptoms
Symptoms that make it hard to go about daily life, go to school or work, be with friends, and take care of important tasks.
Why do some people get PTSD and other people do not?
It is important to remember that not everyone who lives through a dangerous event gets PTSD. In fact, most will not get the disorder.
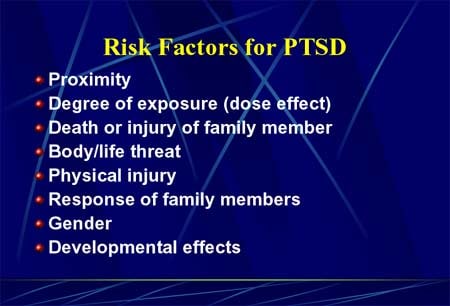
Many factors play a part in whether a person will get PTSD. Some of these are risk factors that make a person more likely to get PTSD. Other factors, called resilience factors, can help reduce the risk of the disorder. Some of these risk and resilience factors are present before the trauma and others become important during and after a traumatic event.
Read the article in Anesthesia & Analgesia.
About Anesthesia & Analgesia Anesthesia & Analgesia was founded in 1922 and was issued bi-monthly until 1980, when it became a monthly publication. A&A is the leading journal for anesthesia clinicians and researchers and includes more than 500 articles annually in all areas related to anesthesia and analgesia, such as cardiovascular anesthesiology, patient safety, anesthetic pharmacology, and pain management. The journal is published on behalf of the IARS by Lippincott Williams & Wilkins (LWW), a division of Wolters Kluwer Health .
About the IARS The International Anesthesia Research Society is a nonpolitical, not-for-profit medical society founded in 1922 to advance and support scientific research and education related to anesthesia, and to improve patient care through basic research. The IARS contributes nearly $1 million annually to fund anesthesia research; provides a forum for anesthesiology leaders to share information and ideas; maintains a worldwide membership of more than 15,000 physicians, physician residents, and others with doctoral degrees, as well as health professionals in anesthesia related practice; sponsors the SmartTots initiative in partnership with the FDA; and publishes the monthly journal Anesthesia & Analgesia in print and online.
About Wolters Kluwer Health Wolters Kluwer Health is a leading global provider of information, business intelligence and point-of-care solutions for the healthcare industry. Serving more than 150 countries worldwide, clinicians rely on Wolters Kluwer Health’s market leading information-enabled tools and software solutions throughout their professional careers from training to research to practice.
Wolters Kluwer Health is part of Wolters Kluwer, a market-leading global information services company. Wolters Kluwer had 2013 annual revenues of €3.6 billion ($4.7 billion), employs approximately 19,000 people worldwide, and maintains operations in over 40 countries across Europe, North America, Asia Pacific, and Latin America.
###