Diagnostic Criteria
All the behaviors you just read about may be symptoms of schizophrenia, although very few patients with schizophrenia exhibit all these symptoms. Instead, most individuals with the disease display a few of these symptoms. The set of symptoms a patient with schizophrenia experiences is called a symptom profile. In order to diagnose someone with schizophrenia, a clinician must determine that the person has exhibited at least two psychotic symptoms for at least six months. This does not mean that the psychotic symptoms must be continually present for six months, but rather that the symptoms have been present more often than not. A brief discussion of each of the five psychotic symptoms follows:
Delusions. A delusion is a false belief that cannot be explained by one’s culture or social environment. Someone with a delusion cannot be dissuaded from this belief, despite evidence that it is not consistent with societal norms.
There are several types of delusions. A delusion of grandeur is one in which the person believes that he or she is someone famous or very important such as God or a movie star.
Alternatively, patients with this kind of delusion might believe that they are especially close to a celebrity or religious figure. Some patients have delusions of guilt in which they believe that they have committed a terrible crime or sin. Someone with schizophrenia might have a somatic delusion in which he or she believes that something terrible has happened to his or her body.
For example, some people with schizophrenia believe they have developed cancer or that their intestines have been replaced with a garden hose. Perhaps the most common kind of delusion is a persecutory delusion.
A person with a persecutory delusion believes that someone or something is trying to hurt him or her. A delusion of reference causes patients to believe that they are being talked about, sometimes on the television or radio, or in the newspaper.
Finally, some patients with schizophrenia experience delusions of thought control, in which they believe that thoughts are being put into or taken out of their minds.
Hallucinations. Hallucinations occur when someone perceives something that others cannot perceive. The most common form of hallucination is auditory, which involves hearing things others can’t hear.
Additionally, hallucinations may be visual, in which people believe they see something that no one else can see. Tactile hallucinations occur when an individual feels something that he or she can’t explain, like the tingling of electricity for no reason. Rarely, schizophrenia patients experience olfactory hallucinations and smell things that other people cannot smell. Finally, few patients experience gustatory hallucinations and taste things that other people can’t taste. The content of gustatory and olfactory hallucinations is usually unpleasant, like the smell or taste of garbage or something rotting.
Disorganized Speech. Perhaps the most puzzling symptom of schizophrenia is disorganized speech. Someone whose speech is disorganized is frequently off-topic and nearly impossible to understand. A patient might start talking about his or her mother and quickly change the subject and begin talking about apple orchards. The connection between the mother and apple orchards is usually only understood by the patient.
That is, the patient may have started thinking of his mother, which led him to think about his childhood home, which was in New York City, which reminded him of the Empire State Building, which reminded him of Empire apples. A patient who is severely disorganized is even more difficult to understand. Someone who speaks in this way may construct a sentence like this, “There is nail polish on the pizza which sits on a truck, good luck!” Not only is this sentence nonsensical, but the last few words rhyme. As in the case study of Emilio, one form of disorganized speech is clang associations, or using rhyme inappropriately. The most extreme form of disorganized speech is called word salad.
This is speech that is so disorganized that it makes no sense at all, literally or grammatically. An example of word salad is, “Run simple cake gate spilling baby.” Interestingly, grossly disorganized speech is so contrary to regular language patterns that it is extremely difficult to mimic. Forming associations between words and objects is a natural behavior. It is so natural that it is nearly impossible to think of words that are completely unrelated.
Disorganized Behavior. In addition to speech, behavior may be disorganized and symptomatic of schizophrenia. Disorganized behavior means that the patient has difficulty with goal-oriented behavior. Patients who have disorganized behavior have problems dressing themselves or preparing food to eat.
They often dress inappropriately, in clothes that are dirty or obviously mismatched. Some people with schizophrenia will go out in the winter in shorts and a T-shirt, or they will dress in a sweatshirt and overcoat in the summer. Other forms of disorganized behavior include shouting or cursing in public.
Negative Symptoms. The final category of psychotic symptoms is negative symptoms. Recall that negative symptoms refer to normal behaviors that some patients with schizophrenia lack. You may remember primary negative symptoms by thinking of the three As. The three As refer to anhedonia, avolition, and alogia. Anhedonia is an inability to enjoy activities, or in general to get pleasure out of life. These patients may have low energy and, as a result, spend a lot of time just sitting around or sleeping.
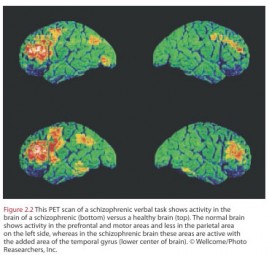 Figure 2.2 This PET scan of a schizophrenic verbal task shows activity in the brain of a schizophrenic (bottom) versus a healthy brain (top). The normal brain shows activity in the prefrontal and motor areas and less in the parietal area on the left side, whereas in the schizophrenic brain these areas are active with the added area of the temporal gyrus (lower center of brain).
Figure 2.2 This PET scan of a schizophrenic verbal task shows activity in the brain of a schizophrenic (bottom) versus a healthy brain (top). The normal brain shows activity in the prefrontal and motor areas and less in the parietal area on the left side, whereas in the schizophrenic brain these areas are active with the added area of the temporal gyrus (lower center of brain).
© Wellcome/Photo Reasearchers, Inc.
Often, patients with negative symptoms are not interested in life in general and have little motivation to try new things. Having little motivation or persistence in beginning or completing tasks is called avolition. Another negative symptom is alogia, or a difficulty or inability to speak.
Patients with alogia are very difficult to treat with therapy because they might never answer a question about how they are feeling or at least take a long time to do so. Patients with negative symptoms are rarely interested in or comfortable around other people. They lack social skills and experience difficulty interacting with others. Many patients with predominantly negative symptoms keep to themselves and withdraw from social activities.
In order to be diagnosed with schizophrenia, a patient must exhibit symptoms in at least two of the categories listed above.
A patient may be diagnosed with schizophrenia, however, if he or she exhibits one of the following three behaviors, even in the absence of other symptoms:
1. If the patient’s delusions are significantly bizarre, such as believing that the FBI is wiretapping one’s apartment and that aliens are performing experiments on the patient at night.
2. When a patient experiences auditory hallucinations in which there are two voices talking to each other.
3. When a patient hears a voice keeping a running commentary on what the patient is doing. This means that the patient hears a voice saying things like, “Now you are going to the store to buy groceries. The woman at the checkout counter is looking at you because she knows you are bad.” Patients who hear a running commentary generally can get little quiet from the voices in their head.
Heather Barnett Veague, Ph.D.
Heather Barnett Veague attended the University of California, Los Angeles,
and received her Ph.D. in psychology from Harvard University in 2004. She
is the author of several journal articles investigating information processing
and the self in borderline personality disorder. Currently, she is the Director
of Clinical Research for the Laboratory of Adolescent Sciences at Vassar
College. Dr. Veague lives in Stockbridge, Massachusetts, with her husband
and children.
References