Opioid Overdose Prevention Programs May Reduce Deaths
Community opioid overdose prevention programs (OOPPs) - including the use of naloxone (Narcan) for rapid drug reversal - can improve bystander responses to overdose of heroin and related drugs, according to a study published in the June issue of the Journal of Addiction Medicine.
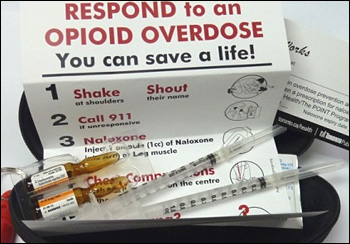
There is growing interest in OOPPs to fight the rising number of deaths from overdose of opioids, including heroin and prescription painkillers. In these programs, kits containing naloxone are distributed directly to patients at risk for overdose. Naloxone kits and training are often delivered in conjunction with needle exchange programs.
Christine M. Wilder, University of Cincinnati School of Medicine, Cincinnati, Ohio, and colleagues identified and analysed the results of 19 published studies evaluating OOPPs. The training programs included recognition, prevention, and risk factors for overdose; and how to respond to an overdose, including naloxone administration. Naloxone was usually given by injection, but sometimes by nasal administration.
Fourteen studies provided follow-up data on more than 9,000 OOPP participants. Nearly half of patients participating in OOPP programs had experienced an overdose during their lifetime, and about 80% had witnessed an overdose.
Eighteen studies provided data on nearly 1,950 naloxone administrations. When naloxone was given in response to an overdose, the person giving it was usually also an opioid user.
Eleven studies reported 100% survival; the rest reported survival rates of 83% to 96%. Two studies provided data suggesting that OOPPs were associated with community-wide reductions in opioid overdose deaths. The studies also provided information on 12 unsuccessful administrations, in which naloxone did not reverse the overdose for various reasons.
Community-Based Opioid Overdose Prevention Programs Providing Naloxone - United States, 2010
Drug overdose death rates have increased steadily in the United States since 1979. In 2008, a total of 36,450 drug overdose deaths (i.e., unintentional, intentional [suicide or homicide], or undetermined intent) were reported, with prescription opioid analgesics (e.g., oxycodone, hydrocodone, and methadone), cocaine, and heroin the drugs most commonly involved. Since the mid-1990s, community-based programs have offered opioid overdose prevention services to persons who use drugs, their families and friends, and service providers. Since 1996, an increasing number of these programs have provided the opioid antagonist naloxone hydrochloride, the treatment of choice to reverse the potentially fatal respiratory depression caused by overdose of heroin and other opioids. Naloxone has no effect on non-opioid overdoses (e.g., cocaine, benzodiazepines, or alcohol). In October 2010, the Harm Reduction Coalition, a national advocacy and capacity-building organization, surveyed 50 programs known to distribute naloxone in the United States, to collect data on local program locations, naloxone distribution, and overdose reversals. This report summarizes the findings for the 48 programs that completed the survey and the 188 local programs represented by the responses. Since the first opioid overdose prevention program began distributing naloxone in 1996, the respondent programs reported training and distributing naloxone to 53,032 persons and receiving reports of 10,171 overdose reversals. Providing opioid overdose education and naloxone to persons who use drugs and to persons who might be present at an opioid overdose can help reduce opioid overdose mortality, a rapidly growing public health concern.
Overdose is common among persons who use opioids, including heroin users. In a 2002–2004 study of 329 drug users, 82% said they had used heroin, 64.6% had witnessed a drug overdose, and 34.6% had experienced an unintentional drug overdose. In 1996, community-based programs began offering naloxone and other opioid overdose prevention services to persons who use drugs, their families and friends, and service providers (e.g., health-care providers, homeless shelters, and substance abuse treatment programs). These services include education regarding overdose risk factors, recognition of signs of opioid overdose, appropriate responses to an overdose, and administration of naloxone.
To identify local program locations and assess the extent of naloxone distribution, in October 2010 the Harm Reduction Coalition e-mailed an online survey to staff members at the 50 programs then known to distribute naloxone. Follow-up e-mails and telephone calls were used to encourage participation, clarify responses, and obtain information on local, community-based programs. The survey included questions about the year the program began distributing naloxone, the number of persons trained in overdose prevention and naloxone administration, the number of overdose reversals reported, and whether the totals were estimates or based on program data. The survey also asked questions regarding the naloxone formulations currently distributed, any recent difficulties in obtaining naloxone, and the program’s experience with naloxone distribution.
 Studies suggested that OOPP training increased bystanders’ knowledge of overdose prevention and risk factors. Training also increased the use of appropriate overdose strategies, although many bystanders continued to use inappropriate strategies as well. Training didn’t seem to increase bystanders’ willingness to call EMS.
Studies suggested that OOPP training increased bystanders’ knowledge of overdose prevention and risk factors. Training also increased the use of appropriate overdose strategies, although many bystanders continued to use inappropriate strategies as well. Training didn’t seem to increase bystanders’ willingness to call EMS.
Many communities have established or are interested in establishing OOPPs to help stem the rising tide of deaths from opioid overdose. However, there are continued questions about the implementation and effectiveness of these programs. So far, research studies on OOPPs have been limited in number and quality.
An accompanying article discusses the experience of establishing an OOPP at 1 substance use disorders treatment centre. The experience highlights some of the challenges to introducing this new approach.
“OOPP participation is associated with overdose reversals, increased knowledge and ability to respond appropriately in an overdose situation, and the ability of non-medical bystanders to safely administer naloxone,” the authors concluded.
 While naloxone is clearly life-saving in individual cases, more research will be needed to establish whether providing opioid users with overdose training and naloxone kits is an effective way to reduce the number of overdose deaths in the community.
While naloxone is clearly life-saving in individual cases, more research will be needed to establish whether providing opioid users with overdose training and naloxone kits is an effective way to reduce the number of overdose deaths in the community.
The authors emphasised the need for well-designed studies to assess the true impact on overdose deaths, how best to integrate OOPPs into current practice, and the benefits of OOPPs at the population level.
###
SOURCE: Wolters Kluwer Health