Researchers find two distinct genetic subtypes in Crohn’s disease patients
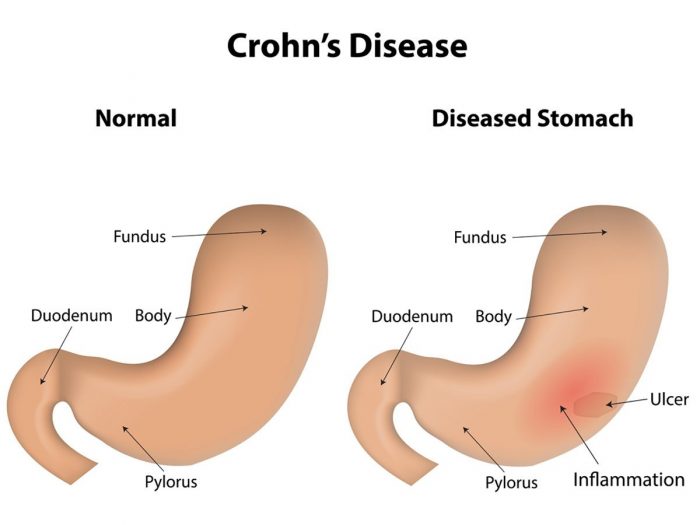
Crohn’s disease, a common inflammatory disorder of the intestinal tract, can have devastating consequences for a patient’s quality of life and is notoriously hard to treat successfully, in part because its course and severity vary so much from one case to the next. Now, UNC School of Medicine scientists have made a discovery that could explain why Crohn’s is so variable: the disease appears to have at least two distinct subtypes, each with its own pattern of gene expression and mix of clinical features.
The discovery, published in the journal Gut, could lead to more effective strategies for treating Crohn’s, which affects close to one million people in the United States. Although people with the disease typically are treated with powerful immune-suppressing drugs, roughly 70 percent eventually require surgery to remove portions of the intestinal tract that have developed blockages or other problems caused by severe inflammation. Even after surgery, the disease often recurs and is therefore not curative.
A deeper understanding of the biology of Crohn’s disease should enable doctors to target it more effectively.
“The one-treatment-fits-all approach doesn’t seem to be working for Crohn’s patients,” said Shehzad Z. Sheikh, MD, PhD, assistant professor in UNC’s departments of medicine and genetics and co-senior author of the study. “It’s plausible that this is because only a subset of patients has the type of disease that responds to standard therapy, whereas, for the rest of the patients, we’re really not hitting the right targets.”
 For the new study, published online today, Sheikh teamed up with Terry Furey, PhD, associate professor in UNC’s departments of genetics and biology and study co-senior author, to map the levels of gene expression in non-inflamed, healthy-looking colon tissue samples taken from 21 Crohn’s patients. When they began looking at the gene expression patterns in these patients, two clear groupings dominated.
For the new study, published online today, Sheikh teamed up with Terry Furey, PhD, associate professor in UNC’s departments of genetics and biology and study co-senior author, to map the levels of gene expression in non-inflamed, healthy-looking colon tissue samples taken from 21 Crohn’s patients. When they began looking at the gene expression patterns in these patients, two clear groupings dominated.
“Although we saw a difference between the Crohn’s samples and samples from people without Crohn’s, we saw an even greater difference at the molecular level between these two subsets of the Crohn’s samples - the healthy tissue from Crohn’s patients and the inflamed samples from Crohn’s patients,” Furey said.
How the two disease subtypes differed was unexpected.
“It was surprising,” said Jeremy Simon, PhD, a research assistant professor in UNC’s department of genetics and co-first author of the study with former graduate student Matthew Weiser, PhD. “Many of the genes that were different between the two Crohn’s subtypes are markers that distinguish the colon from the ileum, despite these being colon biopsies.”
The team described how in one disease subtype, the pattern of gene expression mostly resembled that of normal colon tissue. In the other, gene expression shifted towards the pattern normally seen in the ileum - the part of the small intestine that empties (via a structure called the cecum) into the colon, and is often the first area affected in Crohn’s.
The team looked not only at specific gene expression products in the sampled tissue, but also at indicators of the “epigenetic” state of the tissue DNA - the pattern of molecular switches on chromosomes that effectively permit or repress nearby gene activity. Here, too, there was a distinction between the two Crohn’s subtypes, suggesting that their differences in gene expression stemmed from differences in the basic programming of the affected cells.
The colon samples were from adults with Crohn’s that had all undergone surgery, leaving open the possibility that their treatment and disease histories may have played a role in the observed gene expression patterns. So the team then looked at a recently published gene expression dataset from 201 children with newly diagnosed, never-treated Crohn’s, and although the tissue samples this time were from the ileum, the researchers again observed the same two colon-like and ileum-like disease classes.
“This suggests that these molecular programs or baseline genomic signatures of Crohn’s subtypes exist independently of patients’ ages or treatment histories,” said Sheikh.
Importantly, these two signatures were linked to different patterns of clinical illness. The “colon-like” cases, for example, were more likely to have gut inflammation visible during colonoscopy, rectal disease (notoriously difficult to manage from a clinical standpoint), and severe enough colon inflammation to require surgical removal of the colon (colectomy).
Sheikh, Furey, and their colleagues now hope to translate these results into a diagnostic test on tissue samples from routine colonoscopies, or perhaps even on blood samples. Such tests could help doctors classify Crohn’s patients and choose the best therapies.
As an initial follow-up, they plan a broadened study to confirm their findings in a much larger set of patient samples, a project for which they recently received funding from the National Institutes of Health. They also hope to undertake a long-term study, in which they would test patients for their Crohn’s subtype when they are initially diagnosed with the disease, and then follow them for several years to see whether the assigned subtype predicts the disease course.
“We hope one day to be able to test Crohn’s patients for the subtype of the disease they have, and thus determine which treatment should work best,” Sheikh said. “The idea is to find the best therapeutic course for each patient as quickly and efficiently as possible.”
###
The other co-authors of the study were UNC GI fellow Bharati Kochar, MD; UNC graduate student Adelaide Tovar; UNC postdoctoral fellow Jennifer W. Israel, PhD; former UNC graduate students Adam Robinson, PhD, and Gregory R. Gipson, PhD; UNC research technician Matthew S. Schaner; Hans H. Herfarth, MD, PhD, professor of medicine at the UNC School of Medicine; R. Balfour Sartor, MD, the Midgette Distinguished Professor of Medicine and Microbiology & Immunology and co-director of the UNC Multidisciplinary Center for IBD Research and Treatment; Reza Rahbar, MD, assistant professor of surgery at UNC; Timothy S. Sadiq, MD, assistant professor of surgery at UNC; Mark J. Koruda, MD, professor of surgery; and Dermot P.B. McGovern, MD, PhD, professor of medicine, Director of Translational Medicine, and the Joshua L. and Lisa Z. Greer Endowed Chair in IBD Genetics at the David Geffen School of Medicine at UCLA and Cedars-Sinai Medical Center.
The work was supported by the American Gastroenterological Association, the Broad Medical Research Program, Crohn’s and Colitis Foundation of America, and the National Institutes of Health.
###
Mark Derewicz
.(JavaScript must be enabled to view this email address)
984-974-1915