Fecal incontinence in the elderly
Fecal incontinence (FI), the involuntary loss of formed stool, can be a social as well as a hygiene problem and is often devastating for patients and their caretakers. Current data, which are probably underestimated, indicate that the occurrence is remarkably high. The etiology of FI is multifactorial; risk factors include advancing age, previous obstetric trauma, diabetes, fecal impaction, stroke, and dementia. The management of FI in the elderly depends on etiologic factors. However, there are many treatment options for sufferers of FI including bulking agents, antidiarrheals, anticholinergics, biofeedback, surgery for sphincter defects, and sphincter bulking devices. The appropriate treatment can be guided by a thorough workup of these patients and can result in a significant improvement in quality of life.
Fecal incontinence is an underreported problem in the general population; it is especially common in elderly persons (aged ?65 years) residing in the community or in long-term care settings. It affects more women than men during younger years, but this differential narrows with age. Physiological changes such as sphincter muscle and sensory abnormalities in the anorectal region contribute to this problem, as do factors such as dementia, physical disability, and fecal impaction.
Treatment with biofeedback is feasible in many elderly patients. Those with advanced dementia or physical disability may benefit from a bowel habit training program. Selected patients may require surgical sphincter repair. Minimally invasive techniques such as radiofrequency energy application offer promising future treatment options. The purpose of this review is to provide current information on fecal incontinence and its management.
Roach M, Christie JA. Fecal incontinence in the elderly. Geriatrics. 2008;63(2):13-22.
Key words: elderly, fecal incontinence, biofeedback, treatment
Drugs discussed: analgesics, antimicrobials, cardiovasculars, CNS agents, gastrointestinal agents, theophylline, loperamide, diphenoxylate/atropine, codeine phosphate, cholestyramine/colestipol, estrogen, phenylephrine, sodium valproate, tricyclic antidepressants, amitriptyline, bisacodyl, glycerin, barrier creams
Fecal incontinence (FI) is a socially stigmatizing disease that disproportionately affects adults aged 65 and older. Its true prevalence remains largely unknown because of underreporting, but its predominance in the elderly population is undisputed. Nursing home residents bear the burden of this disease. Furthermore, studies have shown an excess in morbidity among elderly persons with FI living at home. The most effective way to address FI is to identify and treat the etiologic factors. This review focuses on the pathophysiology, diagnosis, and treatment of FI in elderly individuals.
Prevalence
FI is the involuntary leakage of stool or gas from the rectum. Clinical manifestations may range from fecal soiling to complete loss of stool from the rectum. The personal impact of FI is profound and far-reaching because of the social isolation that ensues as an individual’s level of functioning in daily life is governed by proximity to a toilet. This disease frequently results in the institutionalization of the elderly because of the difficulty families experience in coping with the disease. It is a marker of poor health and increased mortality. FI is associated with an increase in depression and anxiety among patients that inevitably results in a true or perceived degradation in quality of life.
The exact incidence and prevalence of FI is unknown because of the reluctance of patients to discuss this disorder and the failure of physicians to inquire about it. Nonetheless, its prevalence varies with the study population, 2% to 17% in community-dwelling elderly, 50% to 65% in nursing home elderly, and 33% in hospitalized elderly.
Double incontinence (FI and urinary incontinence [UI]) has been found to be more common than either entity alone, with 50% to 70% of patients with UI also carrying the diagnosis of FI. This striking concordance of UI and FI suggests a similar underlying physiologic mechanism, which may include damage to the pelvic floor as a result of trauma or surgery, neurologic disorders, functional impairment, or dementia. Multiple studies have shown that dementia and immobility play a contributory role in UI and FI.
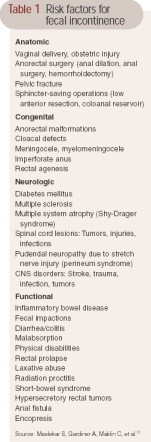 Table 1 Risk factors for fecal incontinence Higher prevalence rates are seen among patients with predisposing conditions such as diabetes mellitus (20%), irritable bowel syndrome (20%), stroke (new onset, 30%; 15% at 3 years poststroke), multiple sclerosis (51%), traumatic spinal cord injury (27%), and spina bifida (80%). These conditions are known to affect mobility as well as cause diarrhea or fecal impaction, all of which are risk factors for incontinence (see Table 1). The higher prevalence among the elderly and nursing home residents may be attributable to clinical and functional factors associated with age such as a higher incidence of constipation, dependence and immobility, cognitive impairment, polypharmacy, and general poor health.
Table 1 Risk factors for fecal incontinence Higher prevalence rates are seen among patients with predisposing conditions such as diabetes mellitus (20%), irritable bowel syndrome (20%), stroke (new onset, 30%; 15% at 3 years poststroke), multiple sclerosis (51%), traumatic spinal cord injury (27%), and spina bifida (80%). These conditions are known to affect mobility as well as cause diarrhea or fecal impaction, all of which are risk factors for incontinence (see Table 1). The higher prevalence among the elderly and nursing home residents may be attributable to clinical and functional factors associated with age such as a higher incidence of constipation, dependence and immobility, cognitive impairment, polypharmacy, and general poor health.
Physiology of continence
Continence is maintained by the integrated action of the structural and functional portions of the anorectal unit, which is comprised of the internal anal sphincter (IAS), external anal sphincter (EAS), striated muscles of the puborectalis (PBR), and intact neurosensory pathways (see Figure 1). Continence is influenced by the consistency and volume of stool delivered to the rectum, the capacity and compliance of the rectum, anorectum sensation, and resting tone. Failure of any component of the anorectal unit may lead to FI when other components/mechanisms are unable to compensate for the defect in the anorectal unit.
The IAS is a 0.3- to 0.5-cm distal continuation of the circular smooth-muscle layer of the rectum. It maintains approximately 70% to 80% of anal resting tone. With increasing age, resting pressure tends to decrease because of gradual degeneration of the IAS. Studies have shown that there is a 30% to 40% decrease in sphincter pressures in adults older than 70 when compared to adults younger than 30. Whether this is attributable to medication or age-related changes in pelvic floor dynamics is unclear. There is evidence that in all age-groups, lower squeeze pressure affects women more than men, with an accelerated diminution after menopause. This may be related to the estrogen-deficient state of menopause, because estrogen receptors have previously been identified in the human stroma and smooth muscles of the anal canal. However, a recent review of the literature failed to show statistically significant gender differences, citing only age-related variation in squeeze pressure.
The EAS is a 0.6- to 1.0-cm expansion of the levator ani muscles (see Figure 1). It circles the IAS and is a tonically active striate muscle that contributes to the remaining 20% to 30% of resting tone. The IAS maintains anal continence at rest while the EAS, PBR, and levator ani assist by voluntary contraction when necessary to maintain continence. The PBR is the proximal continuation of the EAS and it passes posteriorly around the lower part of the rectum to form a sling that creates the anorectal angle. The EAS and PBR are innervated by the distal fibers of the pudendal nerve with some contribution from S4 to the PBR. Progressive neuropathic changes to the external anal sphincter may worsen with aging as evidenced by an increase in length in the motor unit potentials responsible for sphincter contraction. Anal closure is also maintained by the anal mucosal folds and the vascular cushions that expand to keep a tight seal and may contribute 10% to 20% of anal resting pressure (see Figure 1).
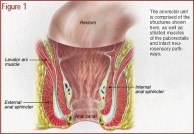 Figure 1 The anorectal unit is comprised of the structures shown here, as well as striated muscles of the puborectalis and intact neurosensory pathways. (Illustration: Kevin Somerville)
Figure 1 The anorectal unit is comprised of the structures shown here, as well as striated muscles of the puborectalis and intact neurosensory pathways. (Illustration: Kevin Somerville)